 |
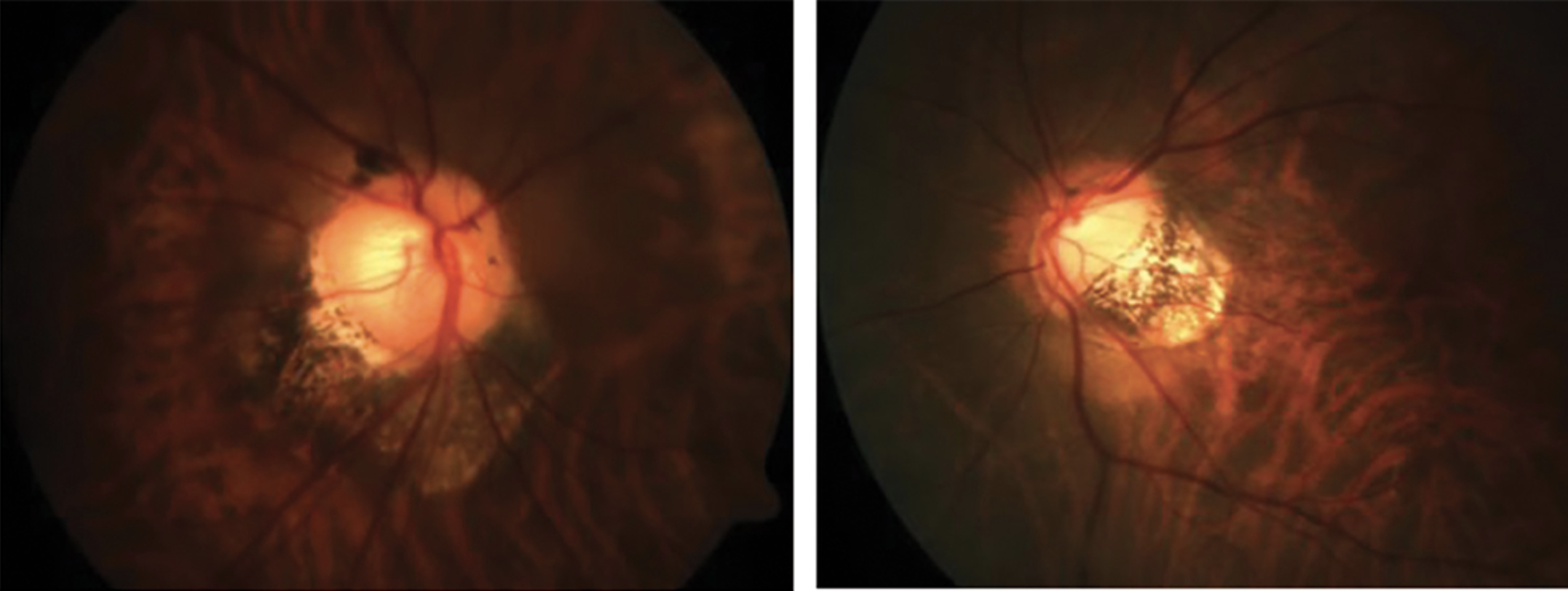
| Myopic maculopathy was almost constant when posterior staphyloma (shown here) were present in this study, agreeing with prior data indicating eyes with this condition have worse visual prognosis. Photo: Andrew Rouse, OD. Click image to enlarge. |
Researchers sought in one new study to determine the nature of the relationship between staphyloma and maculopathy and its development, since this is still unclear. Posterior staphyloma cases were analyzed for the incidence and severity of myopic maculopathy and its repercussions on visual prognosis.
Included in the Spain study were 473 eyes from 259 high myopic patients (70.7% female). Complete ophthalmologic examinations were conducted, under which best-corrected visual acuity (BCVA), axial length, myopic maculopathy classification, presence of posterior staphyloma, pathologic myopia and severe pathologic myopia were determined.
After looking at multimodal imaging, the researchers of the study found posterior staphyloma was present in 69.4% of eyes. These eyes were older, had longer axial length, worse BCVA and greater stage in each of the ATN grading system components, which classifies myopathy according as atrophic, tractional or neovascular. Macular involvement with staphylomas had worse BCVA, greater axial length and ATN. Eyes with pathologic myopia and severe pathologic myopia saw posterior staphyloma presence risk of 89.8% and 96.7%, respectively. Posterior staphyloma was the best predictor of BCVA for myopic patients.
Putting these results together, the authors affirm that “the compound staphylomas and those staphylomas with macular involvement present higher degrees of atrophic, tractional and neovascular myopic maculopathy and, therefore, worse visual acuity.”
Of all the posterior staphylomas, 73.4% were primary. Subtypes by frequency were peripapillary (type III), then inferior (type V), narrow-macular (type II) and wide-macular staphyloma (type I) at 20.1%, 16.8%, 16.5% and 11.6%, accordingly. However, these percentages differ from previous reports that show wide-macular type was the most common, followed by narrow-macular. These differences may be due to ethnicity, since this particular cohort was Caucasian-Mediterranean.
Although several factors have an impact on visual acuity in highly myopic patients, this study found that best predictor for BCVA was the presence of posterior staphyloma, accounting for 12.1% of BCVA variability. What’s more, increased axial length was linked to decreased BCVA, explaining 10.9% of variability. Overall, a 4.6mm increased in axial length would be needed to reduce BCVA similar to the reduction caused by posterior staphyloma presence. Eyes without these staphylomas were most affected in visual acuity by conditions under the neovascular and atrophic components.
The researchers elucidate how posterior staphyloma presence “determines high risk of myopic maculopathy and therefore worse visual prognosis, representing the best predictor for BCVA.”
For clinicians, it is suggested that “posterior staphyloma should be considered practically as a constant hallmark of pathologic myopia and its severe form determining the follow-up and prognosis of these patients.”
Flores-Moreno I, Puertas M, Ruiz-Medrano J, et al. Influence of posterior staphyloma in myopic maculopathy and visual prognosis. Eye. June 26, 2023. [Epub ahead of print]. |

