As eyes treated with pegcetacoplan (Syfovre, Apellis Pharmaceuticals) have been characterized by a significantly slower geographic atrophy (GA) lesion progression toward the fovea, researchers in Italy believed it was important to detect risk factors for the foveal involvement in extrafoveal GA eyes at baseline. Structural OCT is an essential diagnostic tool for the evaluation of individuals with GA as it provides anatomic details regarding the neuroretina and RPE. A recent study assessed the relationship of OCT findings and progression to foveal atrophy in a cohort of eyes with extrafoveal GA and AMD at inclusion. The researchers identified OCT risk factors for two-year foveal atrophy in eyes with untreated extrafoveal GA at baseline.
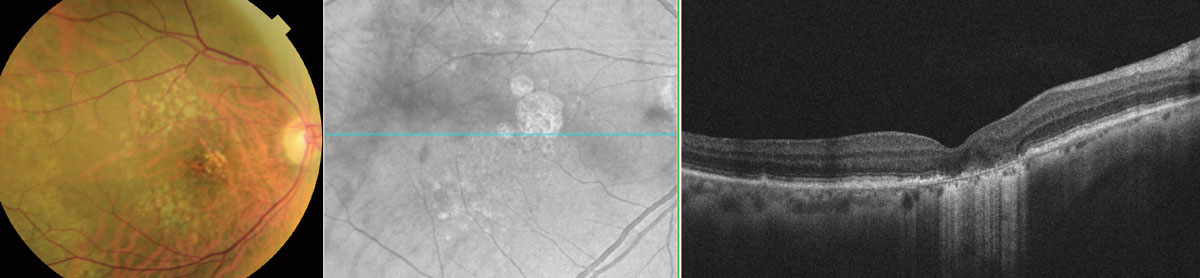 |
| Several imaging risk factors are associated with a higher risk for progression from extrafoveal GA to foveal involvement included lower foveal outer retinal thickness and minimum distance from the foveal central circle and presence of foveal thin double layer sign. Photo: Wendy Harrison, OD, PhD. Click image to enlarge. |
The study retrospectively analyzed 45 participants (45 eyes) with extrafoveal GA at baseline and with two years of regular follow-ups. At month 24, 26 eyes (57.8%) developed atrophy in the foveal central circle, while 11 eyes (24.4%) developed atrophy in the foveal central point.
Significant independent predictive features for the development of atrophy in the foveal central circle included foveal outer retinal thickness (odds ratio; OR: 0.867), minimum distance from the foveal central circle (OR: 0.992) and foveal thin double layer sign (OR: 0.044). The only independent predictive feature for the development of atrophy in the foveal central point was the presence of foveal thin double layer sign (OR: 0.138).
When the foveal central point became involved, a dramatic loss in vision occurred. The researchers are left to believe that the definition of risk factors for the foveal central point atrophy may be clinically relevant.
“Since this was the only independent risk factor for the development of atrophy in the foveal central point, we may speculate that the presumed increase in basal laminar deposits in the foveal region may indicate a more consistent risk factor for the development of atrophy in this region,” they wrote in their paper. “The findings in our study of an increased risk to develop atrophy in the foveal central circle in eyes with a shorter minimum distance from the foveal central circle at baseline may indicate that early changes in the retina surrounding the atrophic lesion may be involving the fovea, this eventually leading to foveal atrophy over time.”
“Assuming that pegcetacoplan-treated eyes are characterized by a significantly slower GA lesion progression toward the fovea, the identification of risk factors for progression toward the fovea is clinically relevant,” the team concluded.
Borrelli E, Barresi C, Berni A, et al. OCT risk factors for two-year foveal involvement in non-treated eyes with extrafoveal geographic atrophy and AMD. Graefes Arch Clin Exp Ophthalmol. February 8, 2024. [Epub ahead of print]. |

