 |
A 69-year-old woman presented as a new patient in June 2024 requesting transfer of her care to our office. Significant in her medical history is bilateral cataract extractions in 2022, followed thereafter with a membrane peel OS. She was discouraged that her vision was suboptimal, she had developed glaucoma and felt the practice she was transferring from did not give her the attention she was looking for. She also felt she was seeing a different doctor each time she was at that office. Eventually, she self-referred to a university eye clinic and apparently was told that she would be able to see somewhat better if her eyeglass prescription was changed, but the last clinic did not agree with that opinion.
Her current medications included only Cytomel (liothyronine sodium, Pfizer) and Synthroid (levothyroxine sodium, AbbVie). She reported allergies to penicillin and cephalosporin antibiotics. Ophthalmic medications included only dorzolamide/timolol combination drops BID OS. Entering visual acuities were 20/30- OD and 20/60- OS through myopic astigmatic correction. Best-corrected visual acuities at this visit were 20/30 OU through a modified spectacle prescription. Pupils were ERRLA with no afferent pupillary defect and extraocular motilities were full in all positions of gaze.
A slit lamp examination of her anterior segments was essentially unremarkable with well-centered intraocular lenses, a clear posterior capsule in the right and an opened capsule in the left. Applanation tonometry at this initial visit was 13mm Hg OD and 10mm Hg OS at 9AM.
The patient was dilated in the usual fashion with phenylephrine and tropicamide. Posterior pole evaluations were significant for small optic discs with small optic cups OU. The retinal vasculature was characterized by mild arteriosclerosis bilaterally and both maculae were characterized by granular retinal pigment epithelium distribution consistent with her age. There was a diffuse epiretinal membrane in the left eye, specifically involving the temporal aspect of the macula. Her peripheral retinal examination was unremarkable.
She declined OCT evaluation of the optic nerves and maculae this visit, stating she would prefer to do these tests after we have had a chance to review her previous records. Certainly, OCT evaluation of the posterior pole is necessary in patients with both retinal disease and optic nerve disease; however, one of her initial complaints was that the previous office, in her opinion, did not “listen” to her when she was in the office. Given this was an initial encounter with the patient, and the doctor-patient relationship per se was not yet fully established, pressing the issue for an OCT at this visit was not necessarily the best option to promote a good and beneficial future doctor-patient relationship. She was certainly willing to transfer her care to us and signed a records release form. As an aside, her husband is a retired physician with whom I’ve worked together with over the years, and she genuinely understands the nuances of medical care.
 |
|
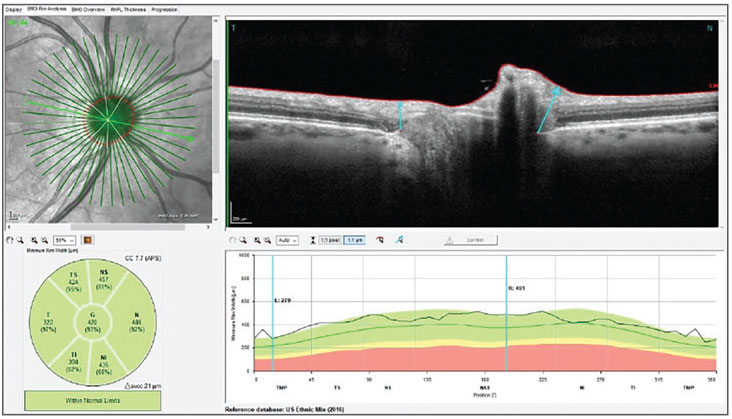
Fig. 1. Bruch’s membrane opening-minimum rim width (BMO-MRW) measurements of the neuroretinal rim in the patient’s right eye. Note the robust neuroretinal rim, small optic cup and slightly small optic disc size. Click image to enlarge. |
At this visit, we opted to not change anything other than her spectacle Rx, as the new refraction did offer some improvement, and to schedule her back in a month, at which time we would hopefully have received her previous records and could proceed with further testing—in particular, OCT. Also discussed was her use of the glaucoma drops in the right eye; perhaps she could switch to a QD regimen, given the healthy appearance of her optic nerves, pending, of course, review of the previous records.
 |
|
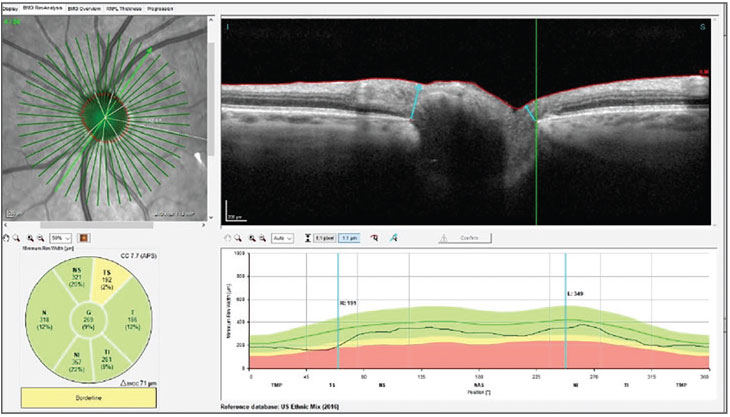
Fig. 2. BMO-MRW measurements of the left neuroretinal rim. Note the slight area of reduced neuroretinal rim thickness in the superior temporal sector of the rim, as highlighted by the green reference line. Click image to enlarge. |
The patient presented again in August 2024 for the follow-up visit as scheduled. At this visit, intraocular pressures were 13mm Hg OD and 12mm Hg OS, and pachymetry readings were 525µm and 531µm OD and OS, respectively. Included here are her optic nerve scans as well as her macula scan of the left eye.
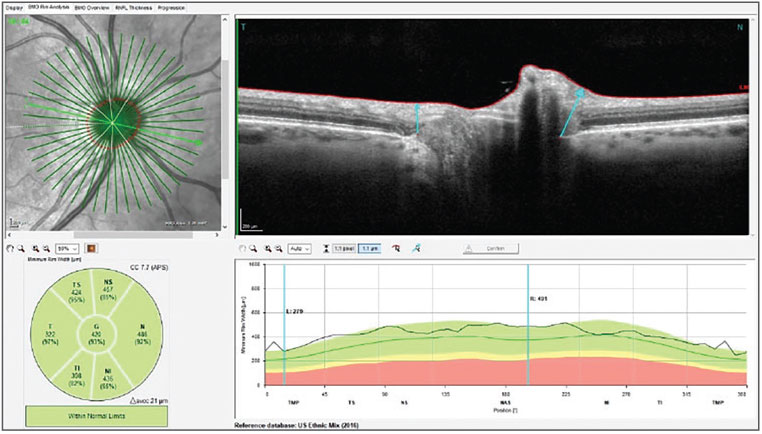
Note in both Figures 1 and 2 a robust and healthy neuroretinal rim in each eye, along with minimal optic disc cupping and somewhat small optic nerve sizes. The only point of interest is in Figure 2, with slight thinning of the neuroretinal rim superotemporally. Figure 3 shows the retinal nerve fiber layer (RNFL) circle scans of the left eye; note specifically slight thinning also in one area of the superior temporal RNFL of the left eye. Note also the statistical thinning of the temporal and inferior temporal sectors of the left RNFL. Keep in mind that the points I am referring to in Figures 1, 2 and 3 are statistical norms based upon the reference database and do not represent frank disease, nor frankly do they represent absence of disease.
 |
|
Fig. 3. Note one small area of slightly thinned RNFL and global thinning of the temporal and inferior temporal Garway-Heath sectors. Click image to enlarge. |
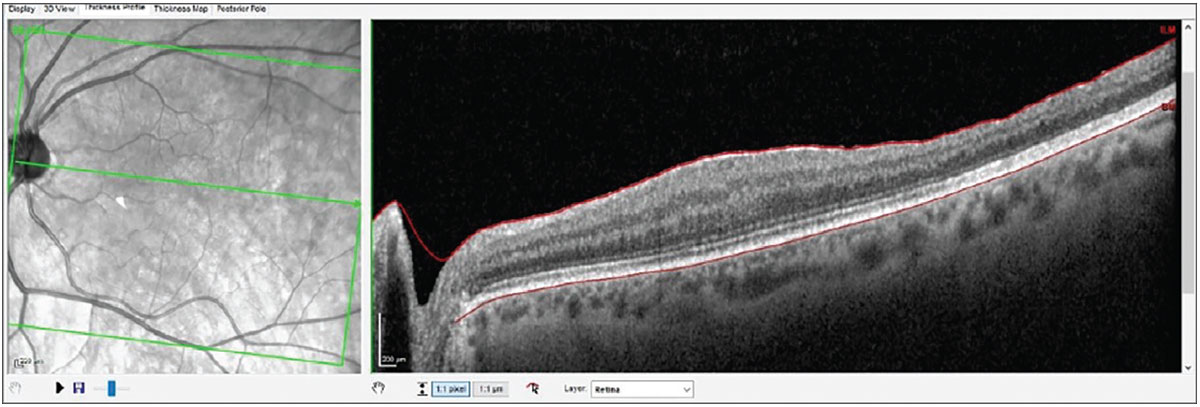
For all intents and purposes, Figures 1, 2 and 3 do not show frank evidence of glaucomatous damage, especially when viewed in conjunction with the optic nerves in stereoscopic examination at the slit lamp. The macula in the left, on the other hand, does show loss of retinal integrity temporally, secondary to the membrane peel, as shown in Figure 4.
 |
|
Fig. 4. Note the normal retinal anatomy on the nasal side of the fovea and the thinned, disrupted retinal anatomy temporal to the fovea, secondary to the membrane peel. Click image to enlarge. |
Discussion
The important takeaway in this case is not so much of a medical decision-making exercise. Rather, it is more of a patient-management exercise. What ultimately brought the patient into clinic were three items: reduced acuity in the left eye, a feeling of not being listened to at the previous office and feeling somewhat herded through said clinic. In reality, on any given day, some of our patients may feel similarly—hopefully, though, not many. While we do get behind in clinic care (especially myself) that each patient in front of us is owed the time and compassion, no matter how many obstacles we face in executing our care. In this case, it happened at another office, and she sought to change to our office.
However, that first visit in situations like this is critical in developing that relationship. While the patient’s vision in the left eye was not optimal (one of the reasons she was seeking our care), that was an easy fix—she simply needed an updated spectacle Rx. Equally important to her, I believe, was her impression of not having the attention from the previous physicians that she thought she deserved. As we know, some people can be unreasonable in their expectations, but she was not one of them. Consequently, the best way to win her over was to give her exactly what she needed: attentive care. “Okay, let’s get your previous records and look at them before we do anything else; okay, let’s wait on the OCT until next visit—not a problem.” These are the words that guided my care plan that first visit.
Now on follow-up visits, we can continue to build that relationship: “I’ve reviewed your records thoroughly; thank you for having them sent to us. They tell us the full picture.” We slowly incorporate more testing on the second visit, all with the attempt to demonstrate to her that she won’t be herded through our office.
Interestingly, her records were in fact telling about her glaucoma diagnosis. Following her membrane peel, which occurred not long after the cataract extraction in the left eye, she developed a steroid response to the prolonged topical steroids she was taking postoperatively and was subsequently medicated with the dorzolamide and timolol combination. After several months and many visits, she was eventually weaned off the steroids, but no one took the time, or perhaps noticed, the lessened need for pressure reduction upon cessation of the steroids.
The discussion with the patient took a natural course at that time: “In reviewing your records, we see that you were on steroids for an extended period and your eye pressures became elevated, thus resulting in the need for the glaucoma medications. However, now that you have been off the steroids for over a year, I think we can begin to taper you off these medications, since that may very well have been a temporary situation.” Words like this that don't disparage other providers but also show the patient you are listening and looking carefully at them go a long way to make them feel comfortable—which is the crux of the doctor-patient relationship.
Moving forward, we’ve asked this patient to stop the dorzolamide/timolol combination and to follow up in a couple of weeks to see how her pressures respond. And at that same visit, we’ll need to do a visual field as well.
There are many ways to lose patients and just as many to gain them. In many instances in clinic, our patient management can be more important than our medical management, but in the long run, both are equally crucial to providing outstanding clinical care.
Dr. Fanelli is in private practice in North Carolina and is the founder and director of the Cape Fear Eye Institute in Wilmington, NC. He is chairman of the EyeSki Optometric Conference and the CE in Italy/Europe Conference. He is an adjunct faculty member of PCO, Western U and UAB School of Optometry. He is on advisory boards for Heidelberg Engineering and Glaukos.

