 |
Q: Is UV exposure in corneal crosslinking (CXL) a contraindication if the patient has a known history of herpes simplex keratitis (HSK)?
“CXL has become an essential tool in preventing progression of corneal steepening in individuals with corneal ectasia, such as keratoconus,” say Sara Stockwell, OD, and Mitch Ibach, OD, of Vance Thompson Vision. The procedure is performed by anesthetizing the cornea, debriding the central 8mm to 9mm, instilling a riboflavin solution, exposing the eye to UV-A light and inserting a bandage contact lens.1
Drs. Stockwell and Ibach note that while the goal of CXL is to prevent further progression of ectasia, many patients experience an improvement in corneal curvature as well, which can lead to improved best-corrected visual acuity.2 They add that CXL is safe and effective when performed correctly; however, as with any ocular surgery, there are complications and adverse effects that can occur, including corneal haze, infection (bacterial/fungal/viral), ectasia progression, best-corrected vision loss, dryness and photophobia.2
CXL Contraindications
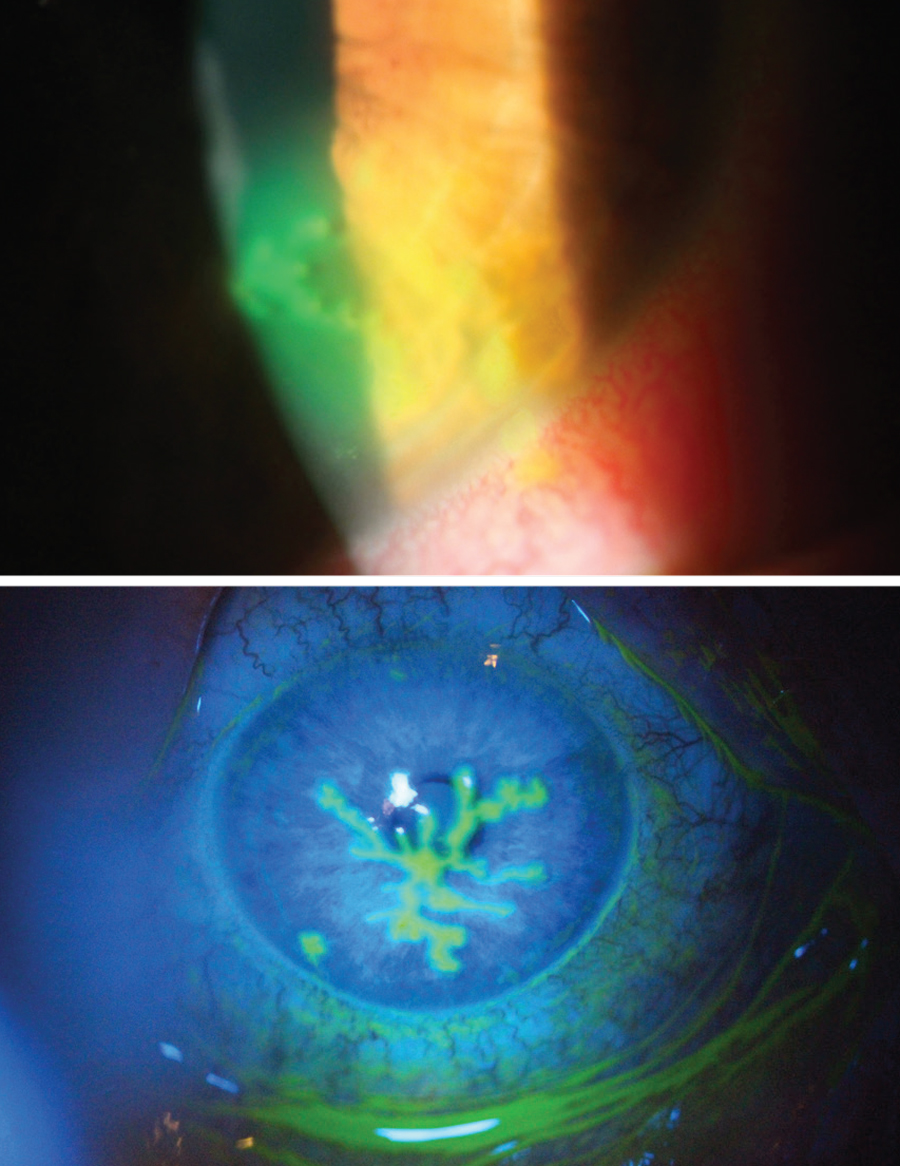 |
| Dendritic HSK with and without cobalt blue filter. Click image to enlarge. |
Some clinicians are leery of recommending CXL to patients with a history of herpes viral infection due to the risk of developing HSK postoperatively, according to Drs. Stockwell and Ibach. There have been reports of HSK infections post-CXL even in individuals with no prior history of HSK.3 It is suspected that exposure to UV-A during the procedure leads to reactivation of the latent herpes simplex virus and subsequent corneal infection, which can occur after any ocular laser surgery likely as a result of stress and/or damage to the corneal nerves.4 In such cases, individuals who were treated appropriately with oral antivirals were not left with any long-term visual or ocular complications, demonstrating the importance of timely postoperative examination to monitor for potential complications.3,4
Despite the risk of developing HSK after CXL, a history of HSK is not always a contraindication for CXL, note Drs. Stockwell and Ibach. If a patient is in need of CXL and has a history of HSK or herpes zoster virus, the doctor duo suggests treating them prophylactically with oral antivirals one month before and six months after the procedure in order to prevent recurrence.3 They typically prescribe valacyclovir 500mg QD to BID or acyclovir 400mg BID. However, if a patient has an active HSK infection, CXL should be postponed until the infection has completely cleared.
The doctors say that, ultimately, the decision to perform CXL should not be hindered by a history of HSK unless a patient has an active infection. The patient and physician should weigh the risks and benefits together to make the best decision. It’s important to remember that HSK can typically be treated effectively and without any serious complications if diagnosed in a timely manner.1 Oral antivirals, which are the most common treatment option for HSK, are safe to use in most healthy individuals.
Dr. Shovlin, a senior optometrist at Northeastern Eye Institute in Scranton, PA, is a fellow and past president of the American Academy of Optometry and a clinical editor of Review of Optometry and Review of Cornea & Contact Lenses. He consults for Kala, Aerie, AbbVie, Novartis, Hubble and Bausch + Lomb and is on the medical advisory panel for Lentechs.1. Al-Qarni A, AlHarbi M. Herpetic keratitis after corneal collagen cross-linking with riboflavin and ultraviolet-A for keratoconus. Middle East Afr J Ophthalmol. 2015;22(3):389-92.
2. Dhawan S, Rao K, Natrajan S. Complications of corneal collagen cross-linking. J Ophthalmol. 2011;2011:869015.
3. Iqbal M, Elmassry A, Badawi AE, et al. Visual and refractive long-term outcomes following standard cross-linking in progressive keratoconus management. Clin Ophthalmol. 2019;13:2477-88.
4. Kymionis GD, Portaliou DM, Bouzoukis DI, et al. Herpetic keratitis with iritis after corneal crosslinking with riboflavin and ultraviolet A for keratoconus. J Cataract Refract Surg. 2007;33(11):1982-4.

