 |
Q: How significant is scleral shape change over time in scleral lens wearers? Will these patients eventually require lens parameter changes?
A: “The shape of the sclera has become an area of increasing interest with the growing popularity of scleral lenses,” suggests Jason Jedlicka, OD, associate professor at the Indiana University School of Optometry and chief of the school’s Cornea and Contact Lens Service. He notes that instrumentation can now measure the sclera in the hopes of achieving better alignment between the lens and the eye. This has raised the question of whether the shape of the sclera changes over time and, if so, if a lens refit is necessary to maintain an optimized fit.
Culprits
While more scientific literature is discussing the shape of the sclera, very little covers changes in this shape, according to Dr. Jedlicka. He says one key consideration to keep in mind when thinking of scleral shape is the overlying conjunctiva, which appears far more vulnerable to short-term changes in thickness, leading to variation in scleral imaging. So, when considering scleral shape change and its relevance to lens fitting, think of the shape of the underlying sclera and that of the overlying conjunctiva as two separate aspects.
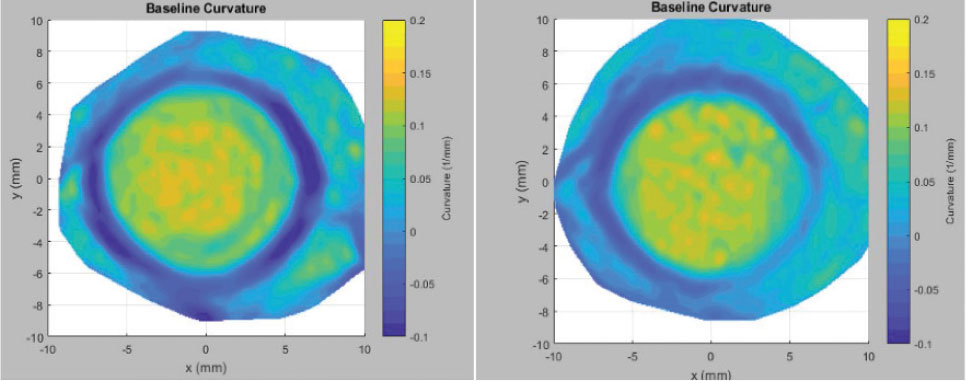
Conjunctival thickness can change in the short term due to compression from contact lens wear, ocular surface inflammation and edema, among other reasons. Conjunctival changes can alter scleral topography, even if the underlying shape of the sclera remains stable.
The conjunctiva can be compressed and thinned due to both scleral and soft lens wear. This compression seems to resolve itself when contact lenses are discontinued for 24 to 48 hours depending on how the lens is fitted and how long it has been worn. The conjunctiva can also thicken due to edema, and this is often seen in corneal gas permeable wearers who show 3 and 9 o’clock staining and injection.
 |
|
Curvature maps of a patient’s sclera just after (left) soft disposable lens removal and 24 hours later. Click image to enlarge. |
In the case of conjunctival thickness changes, to acquire accurate scleral shape imaging for the purpose of lens fitting, lens wear should be discontinued and consideration should be given to treating the ocular surface with topical lubricants or anti-inflammatories to improve conjunctival health.
Scleral shape can also change with corneal ectatic disease. Anatomically, the sclera and the cornea comprise one continuous layer of collagen that has different arrangements of fibers, so the idea that altering the structural stability of the cornea might have a ripple effect on the sclera seems logical.
The Scleral Shape Study Group published a review of 227 eyes with corneal ectasia vs. 115 eyes with normal corneas. The researchers found that the patients with corneal ectasia had more inferior steepening of the sclera with a quadrant-specific effect than healthy controls. While not directly proven by this study, the results seem to suggest that as patients with corneal ectasia progress, their scleral shape can change just as their corneal shape does.1
In addition, there is case-based evidence that collagen crosslinking, which strengthens an ectatic cornea and often creates a degree of flattening, can alter the scleral shape profile as well.2 Therefore, it is reasonable to suspect that disease processes that alter corneal shape by weakening the tissue or procedures that help to strengthen it can also impact the shape of the sclera.
Takeaways
Scleral lenses rest on the conjunctiva, the shape and thickness of which vary noticeably, potentially even day by day. The conjunctiva overlies the sclera, the shape of which changes very little but can be altered over time. Combined scleral and conjunctival shape changes in the short and long term can impact the fit of scleral lenses. Addressing conjunctival health and shape during the fitting period and monitoring for scleral shape changes over time, particularly in the inferior quadrant, allows your scleral lens patients to maintain an optimal fit from the start and enjoy the best experience and outcome possible.
Dr. Shovlin, a senior optometrist at Northeastern Eye Institute in Scranton, PA, is a fellow and past president of the American Academy of Optometry and a clinical editor of Review of Optometry and Review of Cornea & Contact Lenses. He consults for Kala, Aerie, AbbVie, Novartis, Hubble and Bausch + Lomb and is on the medical advisory panel for Lentechs.
1. DeNaeyer G, Sanders DR, Michaud L, et al. Correlation of corneal and scleral topography in cases with ectasias and normal corneas: the SSSG study. J Cont Lens Res Sci. 2019;3(1):e10-20. 2. DeNaeyer G, Sanders D. Collagen crosslinking for keratoconus can change scleral shape: a case report. J Cont Lens Res Sci. 2018;2(1):e15-21. |

