 |
|
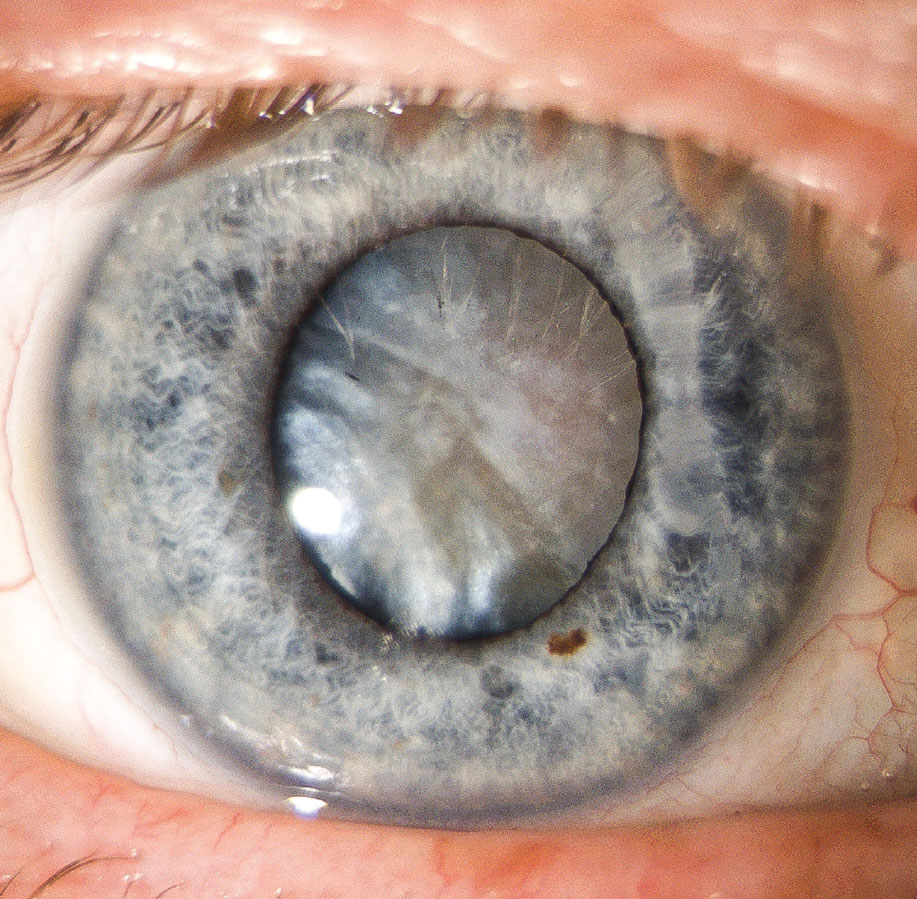
Skilled cataract surgeons were shown to have lower complication rates in uveitic eyes than novices, the study also found. Photo: Gleb Sukhovolskiy, OD. Click image to enlarge. |
Following patients in New Zealand, researchers analyzed both pre- and postoperative risks for this set of conditions. The study—including 471 eyes of 371 subjects—was designed as a retrospective observation. This observation period was extensive, lasting 12 years (2008 to 2020). The outcome measures included additional intraoperative procedures, intraoperative and postoperative complications and postoperative visual outcomes and complications.
Best-corrected visual acuity (BCVA) was measured at first presentation and subsequently after one year, five years, 10 years and at final visit. This measurement was also taken one month, three months and 12 months after receiving cataract operation. Moderate visual loss was standardized as less than or equal to 20/50. Finally, the occurrence of uveitis flares postoperatively was classified as the presence of new uveitis activity, defined as presence of anterior chamber or vitreous cells in a previously quiet eye, or increased activity as increased anterior chamber or vitreous cells requiring increased treatment.
The median duration of uveitis before surgical intervention was 3.0 years, which happened to be a shorter period when compared to prior studies. Additionally, a median period of quiescence before surgery was found to be 1.0 years. Looking at surgery outcomes, researchers found the rate of intraoperative complications to be low at 6.8%. Related to this may be the fact that a high percentage of the primary surgeons were consultants who had already ophthalmology training (82.5%), rather than a fellow or resident surgeon. Preoperatively, the median visual acuity of patients was 20/100, but postoperatively, this statistic rose to 20/50 or better, marking significant improvement in a majority of cases.
With visual acuity rate improving significantly following cataract surgery, it is fair to say that cataract was mainly causing poor eyesight in these patients with comorbid uveitis. Despite this improvement, uveitis relapse following surgery occurred at a rate of greater than 50% in the follow-up period, with the two years following surgery presenting the greatest relapse inflammation rate. This is consistent with previous data reporting relapse rates anywhere from 40.3% to 55.7%.
To combat the risk of uveitic flares post surgery, researchers conclude there should be an absence of intraocular inflammation for at least three months before surgery takes place. This is due to their finding that increased time of disease quiescence was directly associated with reduced risk of flares occurrence.
Uveitic flares were not the only risk after operation, though, as cystoid macular edema (CME) presented in 11.8% of eyes, lower than other uveitic eye studies reporting rates from 12.7% to 27%. A second peak for developing CME was identified at seven months after surgery. For those who developed CME after surgery, this means the prophylactic therapy required to treat it may be needed for a longer period than previously thought.
Considering how quickly cataracts can progress in cases of uveitis, the researchers posit that “earlier surgical intervention in uveitic cataracts has been proposed to minimize the greater surgical risk and difficulties caused by advanced cataracts, as well as to avoid missing posterior segment disease activity and subsequent timely treatment”. When this surgery takes place, clinicians should keep in mind that “postoperative complications can be unpredictable and occur later than expected, so careful monitoring is important to optimize visual outcomes.”
Al-Ani HH, Sims JL, Niederer RL. Cataract surgery in uveitis: risk factors, outcomes, and complications. Am J Ophthalmol. 2022. [Epub ahead of print]. |

