 |
A 14-year-old boy from Jamaica was referred for the evaluation and management of retinal changes discovered in his right eye during a routine eye exam. When he presented a year earlier, everything was normal at that time. He reported no vision problems and says he’s in excellent health and takes no medications. He was born full-term and is the youngest of three siblings.
On examination, his entering visual acuity measured 20/20 OD and OS. His extraocular motility testing was normal. Confrontation visual fields were full to careful finger counting OU and the pupils were equally round and reactive; no afferent papillary defect was detected and his anterior segment exam was unremarkable.
A dilated fundus exam of both eyes showed a small cup with good rim coloration and perfusion in both eyes. The macula appeared normal in both eyes. Changes were noted in the peripheral retina of the right eye (Figure 1). A widefield fluorescein angiography (FA) was performed and is also available for review (Figure 2). The optical coherence tomography (OCT) of the macula was normal in both eyes.
On examination, best-corrected visual acuities were hand movements OD and 20/20 OS, with a prescription of -1.50 +1.00 x 180 OD, -1.75 +1.00 x 005 OS. Her extraocular motility for both eyes was full and extensive. Confrontation visual fields revealed a generalized depression of the right eye, while the left eye was full. Her pupils were equal, round and slowly reactive to light with a 3+ afferent pupillary defect in the right eye.
Color vision measured with Ishihara plates was severely reduced for the right eye only (0/10 OD, 10/10 OS). Her intraocular pressures were measured at 17mm Hg OD and 18mm Hg OS using the Tonopen (Reichert). Anterior segment health revealed 1+ nuclear sclerotic cataract in both eyes. A dilated fundus examination was performed and is available for review (Figure 1). Fluorescein angiography (FA) was also performed and images are available for review (Figure 2).
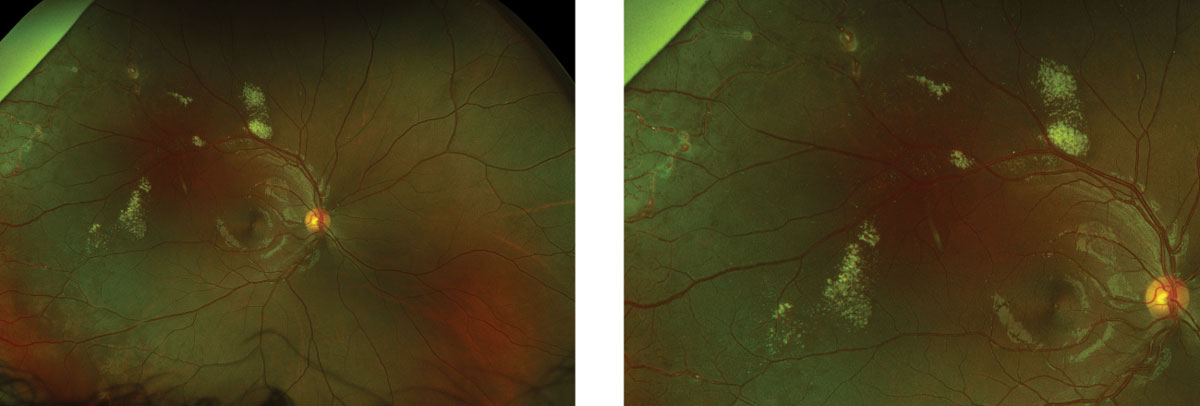 |
| Fig. 1. This wide-angle montage view of the right eye shows peculiar retinal changes. |
Take the Retina Quiz
1. Which best describes the peripheral retinal changes based on the fundus photo?
a. Retinal neovascularization.
b. Aneurismal dilations and retinal telangiectasia.
c. Capillary angiomas.
d. Retinal arterial macroaneurisms.
2. What does intravenous FA show?
a. Capillary dropout.
b. Retinal neovascularization.
c. Quiet choroid with diffuse leakage.
d. Avascular retina with leakage and saccular dilations.
3. What is the correct diagnosis?
a. Resolving branch retinal vein occlusion.
b. Von Hippel disease.
c. Coats’ disease.
d. Sickle cell retinopathy.
4. How should this patient be treated?
a. Observation.
b. Laser photocoagulation.
c. Intravitreal injection of triamcinolone.
d. Intravitreal injection of anti-VEGF medication.
Diagnosis
On the clinical exam, we noted a large area of exudate superior to the arcade, as well as temporal beyond the macula. Beyond the arcades, we noted numerous saccular aneurismal dilated vessels, as well as extensive smaller telangiectatic retinal vessels. The widefield FA highlights the extensive retinal telangiectasia, as well as extensive capillary dropout with peripheral areas of non-perfusion. The good news: even though we saw significant exudate and peripheral ischemia, we saw no exudative retinal detachment or macular edema. Of note, these retinal changes were limited to the right eye; the left eye was normal.
Based on the unilateral retinal changes and the fact our patient is male, our patient was diagnosed with Coats’ disease.
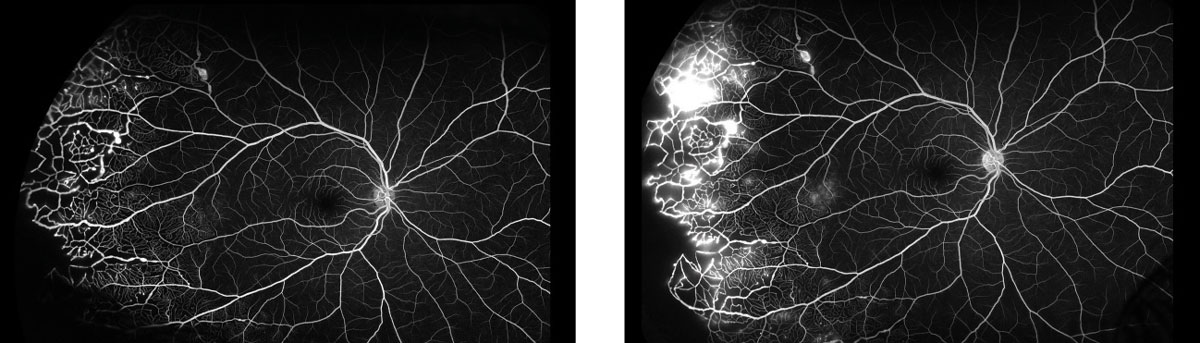 |
| Fig. 2. This fluorescein angiogram shows the patient’s right eye at 29 seconds (at left) and five minutes. |
Discussion
Coats’ disease is an idiopathic vascular anomaly characterized by aneurismal dilations and telangiectasia of the retinal vessels.1-2 It tends to be unilateral and occurs in males 90% of the time during the first to second decade of life.1-2 The retinal capillaries tend to be most affected, but changes can also be seen in the major retinal vessels, particularly the arteries, as was the case for our patient. These vessels leak fluid in the form of exudate. The hallmark of this condition is exudative retinopathy. The extent of involvement and degree of severity can vary.
In milder forms, only isolated areas of the retina may be involved and the prognosis is good. In severe forms, large areas of the retina are involved and patients can present with large amounts of exudate that can lead to an exudative retinal detachment or macular edema.
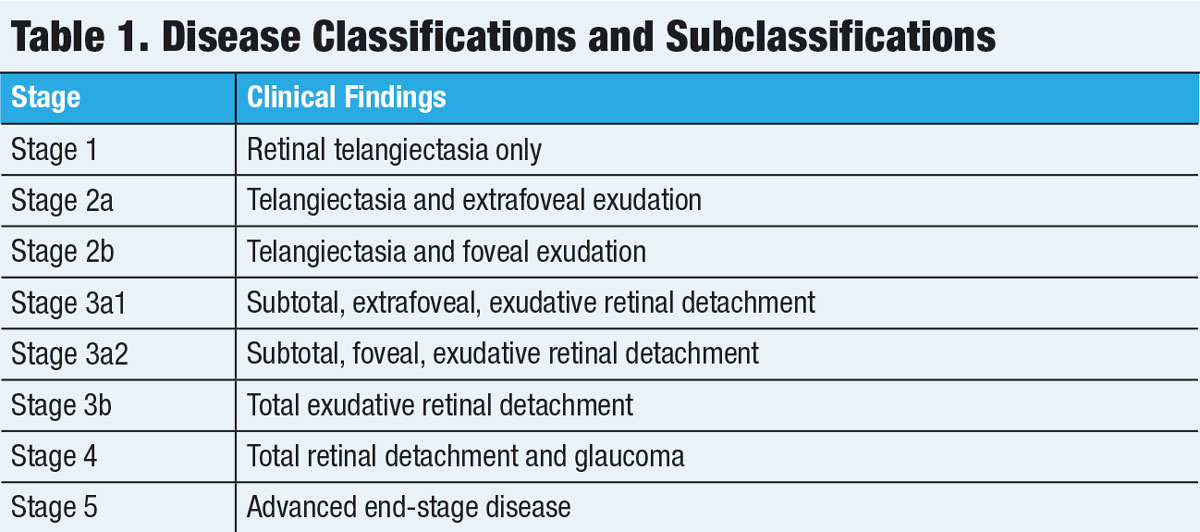
Investigators have stratified the disease into five main stages and further subclassified some stages (see Table 1).3
In a 2001 study of 124 eyes of 104 patients, the visual outcomes were good in stage 1-—with no patients’ visual acuities worse then 20/200 after treatment. In stage 2, 53% had vision worse than 20/200; however, among those with no foveal exudation, only 30% had a poor visual outcome.3 For those with foveal exudation present in stage 2, 86% had a poor visual outcome.3 In patients with stage 3 disease, 74% ended with visual acuity worse than 20/200.3 All patients in stage 4 and 5 ended with visual acuity worse than 20/200.3 Of note, only 18 patients had stage 1 or 2 disease, whereas 106 patients had stage 3 disease or higher by the time they were diagnosed.3
Based on these classifications, our patient would be categorized as stage 2a because no foveal exudation was noted. We expect a good prognosis, especially since he was diagnosed early in the course of the disease.
 |
Treatment
Treatment for Coats’ is indicated if the exudate is extensive and if it seems to be progressive. It is also indicated if central vision becomes affected due to macular edema, or in patients that develop retinal detachment.1 Indirect laser photocoagulation is often a first-line treatment with the goal being to cauterize the affected retinal vessels.4 Laser may also be used to create a barrier between normal and abnormal retina with hopes of sealing off the area of exudation.
Cryotherapy was once a mainstay of treatment but is not used as much anymore except as an adjunct or in more advanced cases. Intravitreal triamcinolone injections has been shown to reduce subretinal fluid and macular exudates and may even facilitate future treatments with laser photocoagulation. Finally, anti-vascular endothelial growth factor therapy may also have great success in reducing subretinal fluid and macular edema but it carries the risk of tractional retinal detachment from the treatment crunch-effect that occurs from regression of neovascularization and scarring that may develop.5 It is, therefore, often reserved for more severe cases.
Vitreoretinal surgery may be required in more advanced cases that do not respond to traditional therapies. Even enucleation may be necessary. In one study, 20 eyes (16%) ultimately required enucleation.3
No immediate treatment was recommended for our patient; instead, he was scheduled to have an examination under anesthesia in approximately six weeks. At that time, treatment with indirect laser photocoagulation or an injection of intravitreal triamcinolone will be strongly considered.
Dr. Jayasimha is an optometric resident at Bascom Palmer Eye Institute in Miami.
Retina Quiz Answers:
1) b; 2) d; 3) c; 4) b.
| 1. Do D, Haller J. Coats’ Disease. In: Ryan S ed. Retina, vol. II – Medical retina. Retinal vascular disease. edited by Schachat. Section 5, Chapter 77. 4th edition St. Louis: Mosby, 2006:1417-23. 2. Gass J. Stereoscopic atlas of macular disease: diagnosis and treatment. 4th edition. St Louis: CV Mosby, 1997:494-582. 3. Shields J, Shields C, Honavar S, et al. Classification and management of Coats’ disease: the 2000 Proctor Lecture. Am J Ophthalmol. 2001;131(5):572-83. 4. Schefler A, Berrocal A, Murray T. Advanced Coats’ disease. Management with repetitive aggressive laser ablation therapy. Retina 2008;28(3 Suppl):S38-41. 5. Kramer B, Ricca A, Blinkley E, et al. Coats’ Disease. Eye Rounds. webeye.ophth.uiowa.edu/eyeforum/cases/237-Coats-Disease.htm. Accessed December 10, 2018 |

