 |
A 54-year-old Hispanic male presented with complaints of blurred vision in his right eye for the past month. The patient has never had eye problems in the past and has always enjoyed good vision.
The patient’s medical history is significant for being HIV positive and having hypertension. He also has had Kaposi’s sarcoma as a consequence of HIV and is being treated with chemotherapy. He is on a host of medications for his HIV and hypertension.
On examination, his best-corrected visual acuity was 20/40 OD and 20/20 OS. Extraocular motility testing was normal. Confrontation fields were full-to-careful-finger-counting OU. His pupils were equally round and reactive to light, with no afferent pupillary defect. His anterior segment exam was unremarkable OU. He had no anterior chamber cells or vitreous cells. His intraocular pressures measured 14mm Hg OU. Dilated fundus exam revealed changes as seen in the fundus photos (Figures 1 and 2). An OCT was performed and is also available for review (Figure 3).
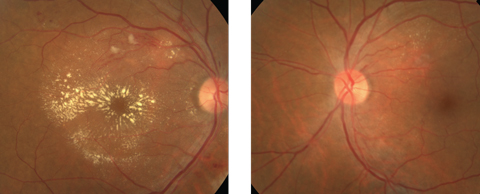 |
| Figs. 1 & 2. Note the obvious finding in the right eye (at left) of our patient, but don’t overlook the finding in the left eye. Click images to enlarge. |
Take the Retina Quiz
1. How would you characterize the macular changes in the right eye?
a. Exudative maculopathy.
b. Macular star formation.
c. Neuroretinitis.
d. Crystalline maculopathy.
2. What additional testing would be most useful in confirming the diagnosis?
a. Fluorescein angiography.
b. Indocyanine green angiography.
c. Blood pressure.
d. Blood serology including indirect fluorescent antibody assay for Bartonella henselae.
3. What is the likely diagnosis?
a. Branch retinal vein occlusion with macular edema.
b. Malignant hypertension or hypertensive emergency.
c. Cytomegalovirus retinitis.
d. Cat scratch neuroretinitis.
4. How should this patient be managed?
a. Referral for anti-viral therapy.
b. Visual field and neuro-ophthalmology consult.
c. Lumbar puncture and MRI.
d. Immediate referral to the ER for blood pressure control.
5. What is the likely visual prognosis for this patient after treatment?
a. Very poor.
b. Moderate.
c. Above average.
d. Excellent.
For answers, see below.
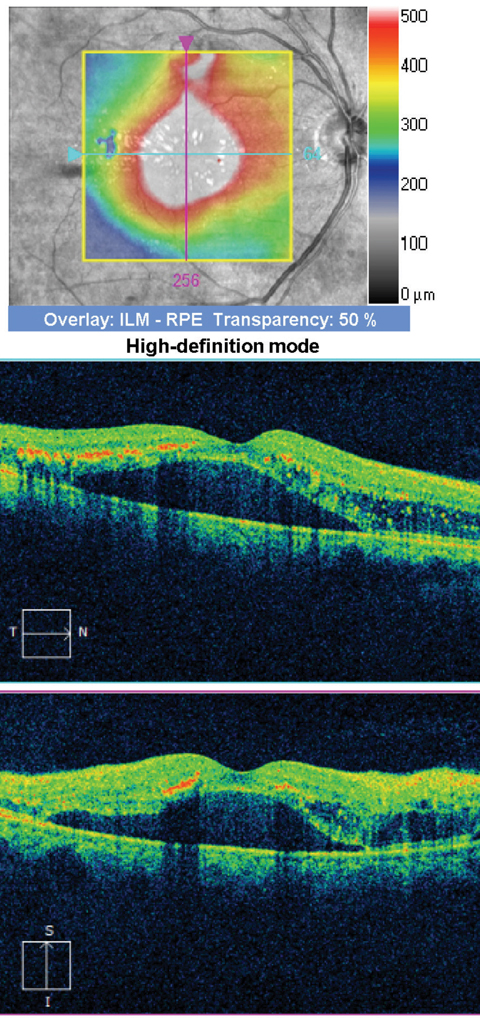 |
| Fig. 3. SD-OCT of our patient’s right eye. Click images to enlarge. |
Discussion
The macular changes that are seen in the right eye represent a macular star. Because of the exudate, our patient also has a neurosensory retinal detachment, as seen on the SD-OCT. In addition, we noticed other vascular-related changes. Superior to the macula, flame hemorrhages and, possibly, a small branch retinal vein occlusion are visible. Also, there is a small hemorrhage nasal to the disc and, in the left eye, there is also a flame hemorrhage superiorly and resolving exudate. So, what is going on with our patient?
The presence of a macular star could be consistent with a neuroretinitis, but there were no vitreous cells, and the vascular changes that are seen in our patient are bilateral. What’s more, when we measured his blood pressure, it was 220/110! Based on the clinical finding and elevated blood pressure, our patient has malignant hypertension, or as it is now more accurately referred to, a hypertensive emergency with end organ damage (eye).
The Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure has provided a classification scheme for hypertension that employs systolic and diastolic criteria. Systolic blood pressure greater than 179mm Hg or diastolic blood pressure greater than 109mm Hg is classified as hypertensive crisis. The condition can be further categorized as either hypertensive emergency or hypertensive urgency.1 End organ damage in the presence of significantly elevated blood pressure is classified as hypertensive emergency, whereas hypertensive crisis occurs in the absence of end organ damage. End organ damage may manifest in the central nervous system, eye, heart (left ventricular dysfunction) and kidney. Hypertensive encephalopathy is associated with severe headaches, change in mental status, transient convulsions, stupor and coma.2
“Malignant hypertension” was used in the past to describe grade IV hypertensive retinopathy including elevated blood pressure and papilledema; however, this term has been removed from National and International Blood Pressure Control Guidelines and is now referred to as hypertensive emergency.2
Hypertensive crisis occurs in approximately 1% of the hypertensive population.3 The presence and extent of end organ damage is related to the level and rate of rise of blood pressure, and the level of underlying hypertensive damage and arterial/capillary change prior to the acute rise in blood pressure. However, organ dysfunction is uncommon with a diastolic blood pressure lower than 120mm Hg.4 It is likely our patient’s blood pressure had previously been even higher than what was measured on the day of his eye exam.
Plan of Action
Our patient presented with a macular star formation and a neurosensory detachment in the right eye as a result of the massive exudate. During a hypertensive crisis, there is a loss of autoregulation of the retinal arterioles, which leads to a breakdown of the blood-retina barrier with leakage of plasma and proteins. Interestingly, our patient didn’t have disc swelling, which is commonly seen with a hypertensive emergency, but that doesn’t mean he didn’t ever have it. In fact, he probably did have disc swelling as evidenced by the flame hemorrhages adjacent to the optic nerve and the resolving exudate in the left eye, but he was in a resolving phase at the time of presentation. It is also interesting to note that the retinal arteries and veins were not significantly attenuated as you would expect to see. In fact, the caliber of the vessels seemed pretty normal, though he did have a prominent arterial light reflex.
Patients in hypertensive emergency must have blood pressure lowered immediately via intravenous infusion of antihypertensive medications in order to avoid further end organ damage and morbidity. Conversely, patients with hypertensive urgency should have blood pressure lowered slowly over 24 to 48 hours with oral hypertensive agents to avoid subsequent ischemia and infarction secondary to the rapid change in blood pressure and loss of arteriole autoregulation.5
Our patient admitted to having poorly controlled blood pressure and, in fact, was having kidney failure. He was sent to the emergency room, but was lost to follow up for more than two years. When he presented again for an eye evaluation, his best-corrected visual acuity was 20/20 in each eye and he had no evidence of the hypertensive emergency two years prior. He is now undergoing dialysis, but his blood pressure is still poorly controlled.
1. The fifth report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1993;153(2)154-83. |

