What's Powering the Next Wave?In the September issue—our 45th annual technology report—find out how AI, telehealth, OCT and other new clinical devices are helping ODs build out their practice for the future. Check out the other featured articles here:
|
Shuttered offices and international pandemic guidelines curtailed in-person patient care in 2020 but also led to demonstrations of sheer tenacity. Despite the challenges, loss and unsteadiness that COVID-19 brought into all of our lives, we would be remiss not to reflect on the opportunities, invention and hopefully lasting patient care innovation that transpired from the events of the last several years. Between social distancing, periods of mandated quarantine and general caution to remain at home, many patients found great utility in virtual communications with practitioners, and doctors were relieved to keep in touch with their patients’ needs.
Immediately upon recognizing the crisis to come, the Centers for Disease Control and Prevention officially began recommending telemedicine in lieu of clinic visits for patients who tested positive for the virus in anticipation of extended periods of social distancing. As a result, practitioners had to pivot their clinical operations—a process that is, in many ways, ongoing.1 Telemedicine is defined by The National Institutes of Health as “the use of electronic information and communication technologies to provide and support healthcare when distance separates the participants.”2 The rapidly evolving modality of care has opened the door to various new doctor-patient interactions.
For example, optometrists became able to advise patients on an incipient chalazion from their own home, diagnose follicular conjunctivitis via video conferencing or review posterior blepharitis treatment algorithms from a quiet, empty office. As practitioners, we all learned to leave our comfort zone by being forced to conduct virtual scheduling and examinations and bill for socially distant patient appointments.
After nearly three years since this nationwide shift towards telehealth, we have benefited from, been challenged by and, eventually, duly accepted this new mode of practice. Here, we will review some lessons worth considering as virtual eye care continues to evolve.
Improving Access to Eye Care
For both patients and doctors, teleoptometry afforded an unparalleled opportunity for patient access. Removing the need for travel allowed more patients to receive direct and expedient access to needed eye care, especially for those in rural locations, with mobility challenges, cost barriers or those who rely on public transportation. During the pandemic, and still now, this was especially vital for patients who were under quarantine, those too nervous to travel and those with comorbidities that more strictly required social distancing. For some physicians, another advantage of this upsurge in telemedicine use was that it helped decrease late and canceled appointments, as well as decreased the number of patients who delayed care, which would potentially worsen their ocular condition.
During this time, it was relieving for practitioners to know that they could still be in touch with their patients and could direct any emergent care, and patients knew that their doctors were never far. One successful example is Northwell Health Physician Partners Ophthalmology Faculty Practice at Manhattan Eye, Ear and Throat Hospital, which allowed for virtual patient care even during the height of the pandemic and in the epicenter of New York City.
Travel aside, virtual visits also removed any potential discomfort during an eye examination from lid eversion, intraocular pressure (IOP) checks or the lasting effects of dilation (not to mention scleral depression or other in-office procedures). The downside, of course, is that these tests, which provide vital information, were not completed. The trade-off for comfort was sometimes bare-bones testing.
Remote telehealth visits at least allowed for basic triage and treatment during a time when access to advanced diagnostics like optical coherence tomography (OCT) or visual field testing was limited. Using even rudimentary examination information, practitioners were able to decide which patients could be managed from afar, or which required in-person follow-up.
Although virtual appointments, for many doctors, vary fiscally in reimbursement from carrier to carrier, it was a massive improvement on an empty schedule and allowed access to funding in order to continue providing care and keep office lights on—literally. Virtual visits also enabled practices to expand available office hours, which made it so that practitioners could open schedules from the comfort of satellite locations.
 |
|
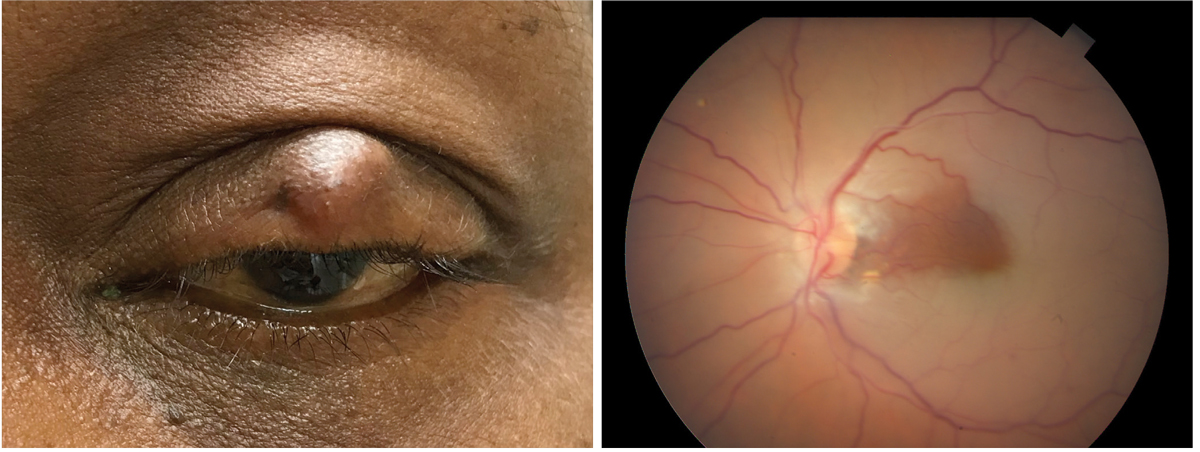
A chalazion (at left) that is easily observable via a video consult is amenable to optometric consult using telemedicine services. By contrast, a central retinal artery occlusion with cilioretinal sparing (at right) is one example of a condition where the presumable complaint of vision loss would necessitate an in-office visit for treatment and diagnosis. Left photo: Joseph Sowka, OD. Click image to enlarge. |
Pitfalls of Technology
New workflows are rarely introduced into a practice without challenges. For patients, teleoptometry requires both reliable internet access and hardware, whether that be a phone, smartphone, tablet or computer. Some existing desktop computers require cameras and/or microphone attachments, in addition to the software needed to sync these devices. Training for both staff and doctors is also a necessity whenever new equipment is added to the office.
 |
|
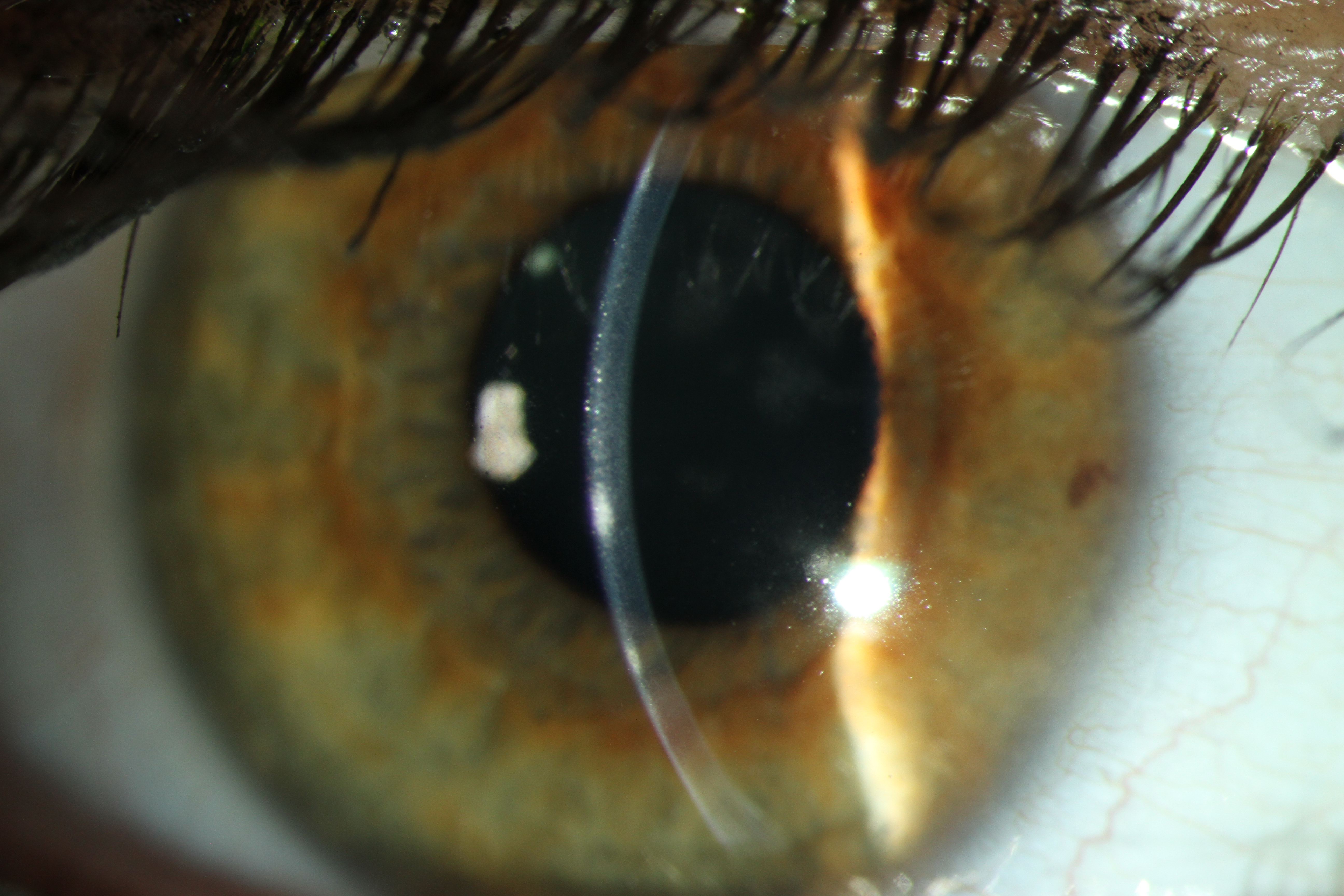
This photo shows a patient with a corneal infiltrate, another condition that would not be treatable via telehealth. Click image to enlarge. |
Regarding access to technology, patients over the age of 50 are often less likely to have access to video conferencing capabilities.3 This is especially pertinent for optometry, as studies have shown that the largest segment of our patient base is between 50 and 64 years old.4 Luckily, as social distancing protocols have loosened in a majority of the country, caregivers or friends have a greater ability than they did two years ago to assist patients with their telehealth technology challenges at home.
Another challenge is that, presbyopia aside, many eyecare patients may not have optimal vision to operate a smartphone with small buttons and icons. In fact, a 2021 American Medical Association (AMA) Telehealth Survey Report, which surveyed over 2,000 ophthalmologists from November through December 2021, revealed that 54% of practitioners cared for patients who experienced technological challenges.5 Notably, 18% of physician respondents reported that they themselves have had to navigate difficulties with telehealth/technology-related workflows and 22% with integrating this new modality of care with electronic medical records (EMR).
If your practice can afford to hire an IT assistant, they could be an asset by ensuring the staff is well-versed in the new equipment, and they can also be a resource for questions or concerns that arise after your team dives into the telehealth workflow. In addition, many academic medical centers offer free online training videos on various topics—e.g., telehealth billing, ethics and risk management, as well as HIPAA compliance—that can serve as an adjunctive method of staff education.
These hurdles on both the patient and practitioner sides—mainly regarding technology access and staff and patient training and education—need to be addressed to keep up with the increasing demand for telehealth services. The AMA survey results showed that 85% of respondents reported using telehealth and 93% of those physicians said they were conducting live, interactive video visits. In order to get those numbers up to 100%, we need to continue to find ways to ensure optometrists can offer effective, universally accessible virtual care to every patient regardless of technological skill. If patients do come to the clinic for occasional in-person appointments, you could take a minute to show them how they can log in for a virtual visit (i.e., via a video conferencing website) and confirm that they know how to do it.
What About Reimbursement?
Let’s talk money. Under the 1135 Centers for Medicare and Medicaid Services (CMS) Waiver Expansion of 2020, many patients, at least at the height of the pandemic, were waived cost-sharing for telehealth visits paid for by federal healthcare programs.6 To boot, patient copays were often waived up front, which helped during what many experienced as a financially trying time.7 From a patient standpoint, this helped improve access to care by removing the requirement of an initial cost. From the practitioner’s standpoint, while helpful, reimbursement became more of a challenge.
From the previously cited AMA survey, lack of insurer coverage of telehealth services afflicted 76% of respondents and 64% cited low or no reimbursement.5 Complicating factors were that telemedicine rules and regulations varied both by state and by individual contracted insurance companies, as well as the mode and technology by which it was performed (i.e., voice vs. video). Telehealth Current Procedural Terminology (CPT) codes are based on how care is delivered, which could either be via video calls face-to-face or through technologies that collect and store images to transmit and interpret later (i.e., sending a photo) or simply audio communications. Modifiers that designate the location of the practitioner from ‘in-office’ to ‘virtual’ are important, as they are reimbursed differently. The American Academy of Ophthalmology created a succinct coding update summarizing which CPT codes were reimbursable, as well as how to accurately specify a telephonic versus video visit, out-of-office locations, modifier applications and hybrid examination.
Additionally, the CARES Act, effective from March 2020, mandated that telehealth visits be paid for at the same rate as in-person visits for those insured by Medicare. The majority of insurance plans followed CMS recommendations following the 1135 Waiver expansion and the CARES Act.8 However, as not all insurance plans followed CMS/Medicare billing guidelines, there was a variety of reimbursing rates on the same telemedicine and virtual care codes.
To complicate matters further, the billing requirements for telemedicine can vary within the same payer by individual insurance plan. This saddles the practitioners’ office with the burden of determining the specific billing requirements for each contracted insurance plan, and verifying the patient’s coverage and benefits.
Luckily, the Telehealth Extension and Evaluation Act was introduced in April 2022, which extends Medicare-enabled telehealth capabilities for two years following the COVID-19 pandemic including continued reimbursement in rural locations, limitations on payments for tests and equipment and remote access to prescriptions.9 This is all to say that although the reimbursement was a complicated algorithm of regulations and rules, for many it was still income-generating and additive for office function.
Note that it is critically important to stay up to date on your state’s reimbursement policies, as these rules are constantly evolving and have already since the beginning of the pandemic.
Preparing for Telehealth’s Future
As a generalization, it could be said that both patients and practitioners are expecting telemedicine to continue as a modality of care, at least in some capacity. Many insurance companies also expect demand for virtual care to remain high post-pandemic. According to Cigna, prior to the pandemic, virtual care made up less than 1% of visits for many subspecialties. At the time of this article, Cigna reported that 25% of visits were completed virtually.10 This shift is expected to continue, with a recent Evernorth survey finding that 75% of Americans see a future that includes obtaining health care from home.11 Thus, looking forward, it’s safe to say that televisits are likely here to stay. The American Optometric Association’s 2020 policy statement echoes this position and further posits that, as doctors of optometry, we must take an active and proactive role in the evolution of telemedicine technology and use.12
Here are four factors to consider for the future of virtual eye care.
1. New ways to access advanced testing for higher-level diagnosis are being developed. With regular iPhone and Android photo software updates, as well as a rapidly changing landscape of smartphone camera hardware, there may be improved near-term focus on smartphone cameras or attachments for self-photography for anterior segment pathology documentation.
There are already many applications that allow for patients to check both near and distance vision, as well as color vision, near point convergence and diplopia. Opportunities down the road involve remotely controlled slit-lamp devices, smartphone-driven nonmydriatic fundus cameras and remote-operated OCT machines in public areas. A few already approved by the FDA include two artificial intelligence designs: IDx-DR (Digital Diagnostics) and EyeArt (Eyenuk) for detecting diabetic retinopathy, ForeseeHome (NotalVision), an at-home neovascular age-related macular degeneration (AMD) monitoring device and program, and Alleye (Oculocare Medical), a free mobile app for self-monitoring AMD progression. Comparing results using self-monitored technology, as opposed to during an office visit, should be completed for integrity in remote testing, but certainly presents an opportunity for advanced diagnostics. For example, home tonometry has seen exciting innovation in recent years as a tool for remote glaucoma care. With these self-monitoring devices, such as the iCare Home tonometer, doctors are able to more closely observe IOP patterns through more frequent testing, which would otherwise only be performed sporadically during in-person visits.
To address the deficiency of remote high-level testing, some larger hospitals are test-driving mobile units with advanced diagnostics (examples include Rutgers University and Duke Ophthalmology). These modified vans have been equipped to screen patients on various machines, including autorefractors, nonmydriatic fundus cameras and OCTs. It is important to recognize and to remind our patients that these remote screening technologies are considered adjunctive to telemedicine treatment and do not replace services performed by a doctor.
 |
|
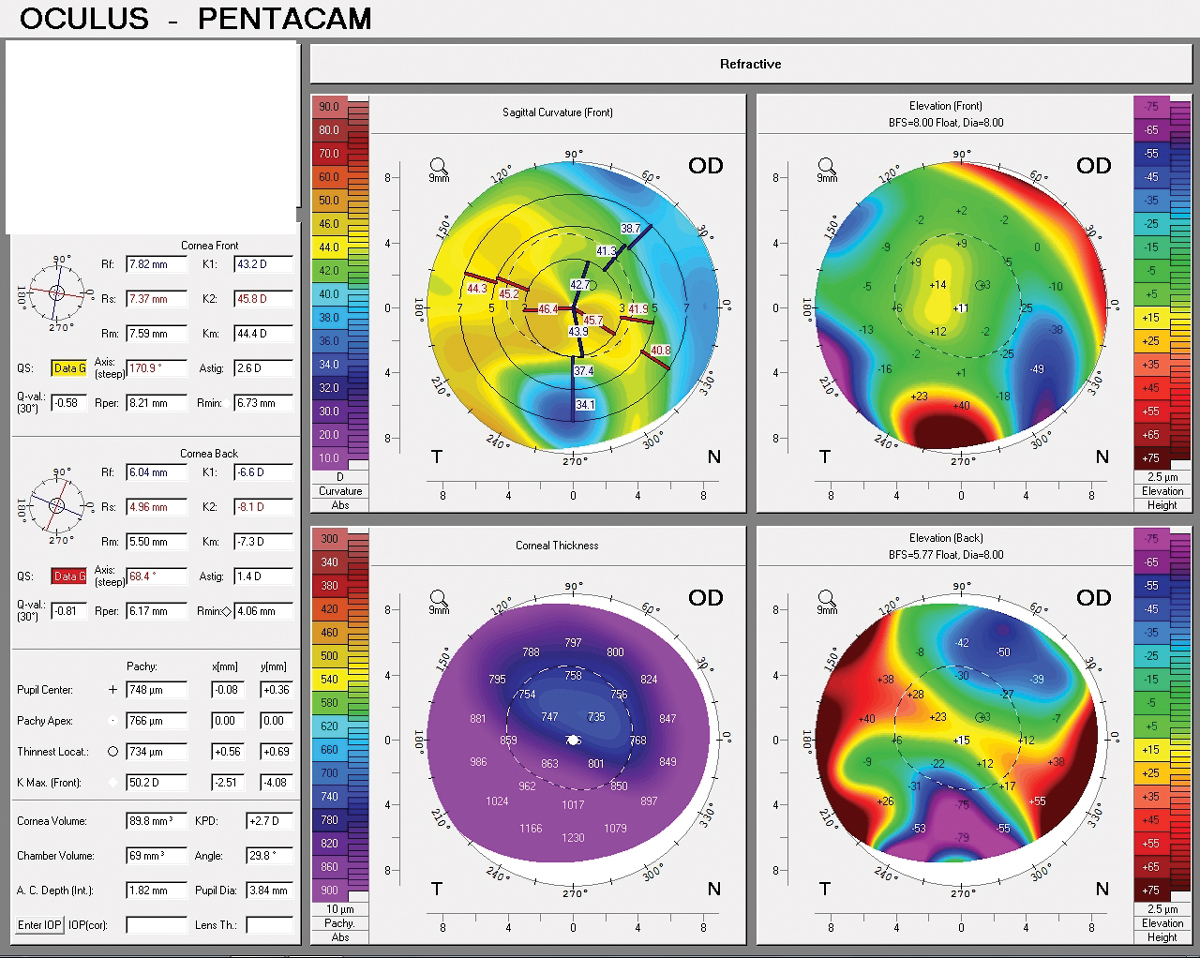
Pentacam of a post-LASIK inferior Salzmann’s nodule, which can only be diagnosed virtually if topography is able to be completed remotely, such as via a mobile testing van. Click image to enlarge. |
2. There is a learning curve to new technology. Incorporating new devices or software efficiently into your practice flow involves consideration of things like schedule rearrangement, office-wide EMR training and designation of hardware devices for data storage. Training technicians and staff to input virtual intake information into the EMR over a secure line and scheduling the practitioner to complete a virtual examination is paramount. Thanks to the capabilities of telehealth, this could be done before, during or after hours. Training of advanced clinical providers and special testing professionals to augment the practitioner’s schedule would extend the telehealth reach.
A practice may find that they need to build a schedule that allows for flexibility to balance in-person and virtual slots and potentially open up appointments after hours to catch up on patient backlogs. Empowering patients to complete remote testing (e.g., self-checking vision, completing an Amsler grid test, compiling all complaints) prior to the start of their appointment will also help with time efficiency.
3. Legislators must support and advocate for fair reimbursement. There is an increasing call for continuing billing flexibilities afforded by the CARES Act, on a permanent basis. Aside from the relaxation of regulatory restrictions afforded by the Telehealth Extension and Evaluation Act, optometrists need continued reimbursement algorithms that align with in-person care and allow telehealth visits to become an extension of in-person visits. In addition, leniency on interstate licensure, or at the very least easily understandable policies and compacts, will be integral for patient access. The US Department of Health and Human Services agrees with this notion, as its website states that interstate compacts would simplify cross-state telehealth by expediting the licensing process or allowing members to practice under a single multistate license.13
4. The range of potential applications for telehealth is broad. As optometry historically moves towards more systemic treatment and collaborative work with other medical subspecialties, virtual visits may accelerate this pursuit by allowing us to virtually consult in emergency departments without leaving our offices as well as collaborate with primary care practitioners, internists, nutritionists and neurologists. In some ways, telehealth is virtually opening the door for us to add value in innumerable medical spaces, in addition to expanding our ability to see our existing patient base.
In sum, telehealth, in its various forms, is here to stay. We may need to adapt our practices, embrace new technology and re-imagine care models as we once knew them. It will be important to continually analyze and compare remote levels of care to in-person visits to ensure that we are providing the same standard of care.
This rapid evolution of virtual healthcare will afford optometrists new ways to offer high-quality care to innumerable patients—one of the few positive pandemic sequelae.
Dr. O’Grady recently began a new role as a division administrative director in the Department of Surgery at the University of Colorado School of Medicine. Prior to the move to Denver, Dr. O’Grady practiced at Northwell Health in New York City. She is a fellow of the American Academy of Optometry and chair of the Membership Committee. She has no financial disclosures.
1. Centers for Disease Control and Prevention. Get your clinic ready for coronavirus disease 2019 (COVID-19). Updated February 25, 2021. www.cdc.gov/coronavirus/2019-ncov/hcp/clinic-preparedness.html. Accessed April 18, 2022. 2. Medicaid.gov. Telemedicine. 2020. www.medicaid.gov/medicaid/benefits/telemedicine/index.html. Accessed April 18, 2022. 3. Pasquinelli MM, Patel D, Nguyen R, et al. Age-based disparities in telehealth use in an urban, underserved population in cancer and pulmonary clinics: A need for policy change. J Am Assoc Nurse Pract. 2022;34(5):731-37. 4. Statistica. Share of Americans who visited an optometrist in the last 12 months in 2018, by age. Published October 24, 2018. www.statista.com/statistics/228528/people-who-used-an-eye-examiner-optometrist-usa. Accessed April 20, 2022. 5. American Medical Association. 2021 Telehealth Survey Report. www.ama-assn.org/system/files/telehealth-survey-report.pdf. Accessed April 20, 2022. 6. Centers for Medicare and Medicaid Services. 1135 Waiver. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertEmergPrep/1135-Waivers. Accessed May 26, 2022. 7. AHIP. Health Insurance Providers Respond to Coronavirus (COVID-19). www.ahip.org/news/articles/health-insurance-providers-respond-to-coronavirus-covid-19. Accessed June 7, 2022. 8. AHIP. Health Insurance Providers Respond to Coronavirus (COVID-19). Published April 27, 2021. www.ahip.org/news/articles/health-insurance-providers-respond-to-coronavirus-covid-19. Accessed August 12, 2022. 9. United States Congress. H.R.7573 - Telehealth Extension and Evaluation Act. www.congress.gov/bill/117th-congress/house-bill/7573/text?r=1&s=1. Accessed June 7, 2022. 10. Cigna. The Four Biggest Health Care Trends of 2022 and How They Impact America’s Employers. newsroom.cigna.com/4-biggest-health-care-trends-2022-impact-on-employers. Accessed June 29, 2022. 11. Evernorth. Virtual Care and Digital Health Are Here to Stay. Published May 4, 2021. www.evernorth.com/articles/virtual-care-and-digital-health-are-here-to-stay. Accessed June 1, 2022. 12. American Optometric Association. AOA spearheads conditions for evolution of telemedicine technology. Published October 22, 2020. www.aoa.org/news/advocacy/patient-protection/telemedicine-policy?sso=y. Accessed August 12, 2022. 13. Department of Health and Human Services. Telehealth Licensing requirements and interstate compacts. Updated March 25, 2022. telehealth.hhs.gov/providers/policy-changes-during-the-covid-19-public-health-emergency/telehealth-licensing-requirements-and-interstate-compacts. Accessed August 12, 2022. |