41st Annual Technology ReportFollow the links below to read other articles from annual update on technology: OCT-A for AMD, Diabetes and Beyond Reality Check: Protecting Ocular Health from Headset Hazards |
With more business threats emerging by the day—including online ophthalmic product sales, remote vision testing, greater regulatory burden, increasing costs and the deluge of new OD graduates—it is more important than ever for optometrists to get the most out of their practice.
The first step is resourcefully finding the most efficient office workflow, which could include everything from spending money on the greatest bang-for-the-buck to reducing wasted motion, eliminating double entry of data and ensuring staff productivity. Using new technology, such as electronic health record systems (EHRs) and new diagnostic devices, can help.
Two decades ago, optometrists were regularly using paper records, manual keratometers, direct ophthalmoscopes and rigid contact lens polishing units. While these aren’t extinct, they are well on their way to joining tangent screens and Schiotz tonometers in the optometric boneyard. Doctors are now bringing new diagnostic technology—such as meibography, specular microscopy, optical coherence tomography angiography (OCT-A), fundus autofluorescence imaging, pattern electroretinogram (ERG) and macular pigment optical density—into their practice for a multitude of reasons. These new technologies can improve the medical care, create a new revenue stream, elevate the patient experience or enhance efficiency, or a combination of all of these.
But sometimes the most important technology has nothing to do with diagnostics. An office management system is often at the heart of today’s optometric practice, and it can make or break the experience for patients, clinicians and staff alike. Let’s take a closer look at how newer technologies can boost practice efficiency and keep your practice booming.
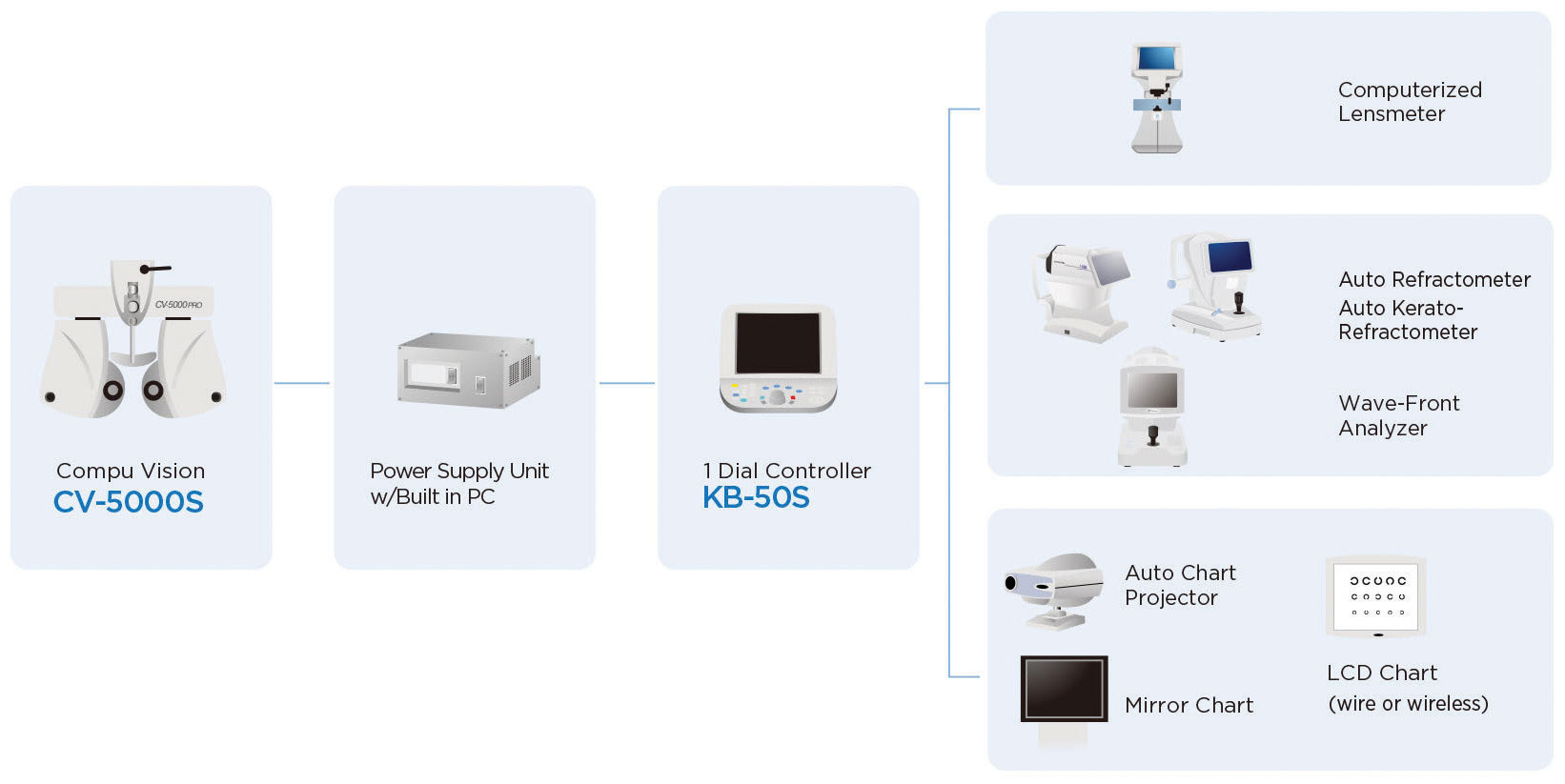 |
| Fig. 1. This chart shows communication between various instruments in an automated refraction system. Click image to enlarge. Image: Topcon Medical Systems |
Proceed with Caution
One of my former practices offered patients ultra-widefield retinal imaging, macular pigment density measurement and retinal nerve fiber analysis—all advanced technology, even by today’s standards. Each measurement was offered to patients for an additional fee during preliminary testing. However, patients balked at having to elect these “a-la-carte” services at a high price, which inevitably caused operational inefficiency.
In retrospect, the fallacy was that this approach created choice overload for the patient; they felt they were being pressured and nickeled-and-dimed. The patient had to discern what was unnecessary and what had compelling value for their health, burdening staff and doctor time that could be better spent elsewhere. Asking the patient to choose whether to have three additional tests created eight different permutations of selection and caused an inconsistent workflow and more errors when charging the patient.
As this example shows, advanced diagnostics alone are not enough; they must also be orchestrated well. When multiple elective tests exist, consider bundling them together rather than having your staff sell each one individually. Alternatively, build them into your exam at no additional fee. Removing patient choice inherently creates greater efficiency with fewer moving parts that can fail.
My current practice, for example, provides digital retinal imaging and fundus OCT for all patients during their routine examination for no additional cost. This creates consumer surplus and elevates their level of care with absolute consistency. The resultant efficiency means I can spend more time discussing the results and giving treatment recommendations. Although across-the-board retinal imaging and OCT are novel, I believe it will eventually become commonplace, if not standard in our industry.
Repetition = Opportunity
Futurists have projected that artificial intelligence and robots will one day take away jobs. If this becomes a reality, the consensus is that the most exposed jobs are those that are “routine, repetitive and predictable.”1 In the same way, tasks within the optometric practice that fit such a description arguably present the greatest opportunity for using EHR and new diagnostic technology to bring greater efficiency.
Thinking through the patient cycle can help you identify several such opportunities, from scheduling and appointment confirmations to patient in-take and case history, preliminary exam measurements, the examination, prescription fulfillment and ordering, billing and collections and post-encounter administration such as delivery notifications and surveys.
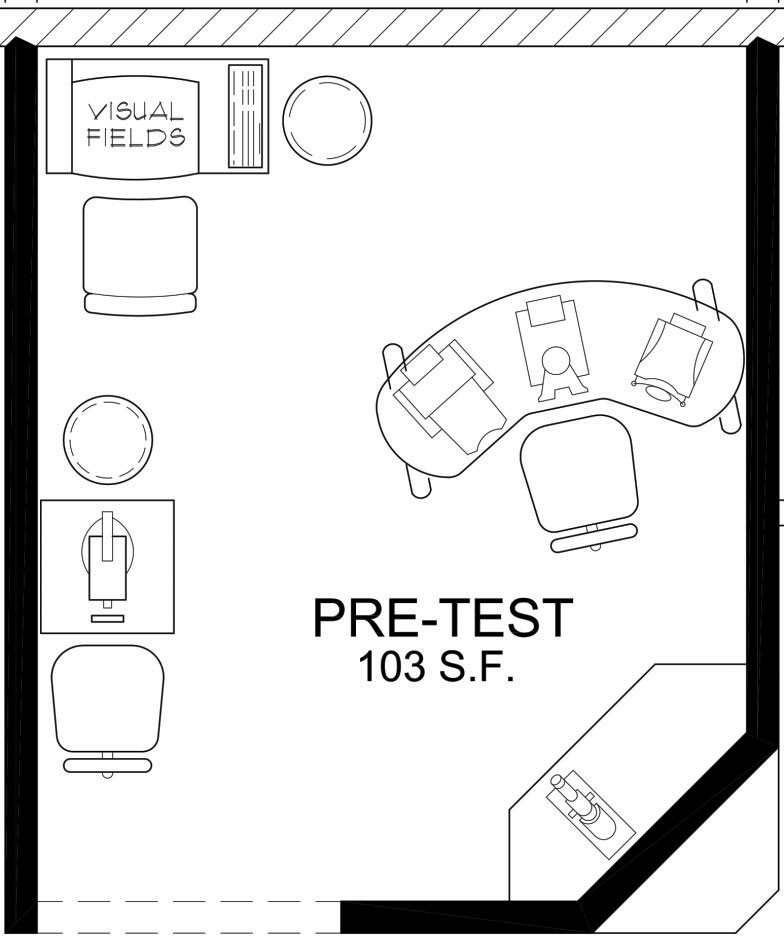 |
| Fig. 2. A proposed layout of diagnostic instruments in a pre-test area. Space planning can optimize function and flow. Image: Eye Designs Group |
System Check
The backbone of any modern optometric practice is the computerized system for recording patient demographic information, scheduling, payment history and exam findings. Today, with more than 40 EHRs available in our industry, optometric practice owners have many choices to pattern their workflow. Which EHR to use is a critical, but rarely easy, decision. Each EHR requires a significant investment in time and money for training and implementation.
After using four different EHRs extensively, I know first-hand that the wrong EHR can create massive inefficiency, but the right one can boost efficiency. The EHR in my previous practice (implemented by a private equity–funded consolidator) tripled the number of mouse clicks required to complete an examination. A poorly matched EHR gratuitously hinders your ability to interact with the patient, forcing you to increase your level of interaction with the computer instead. Conversely, efficient technology frees up more time you can spend with your patient.
If you’re searching for the right EHR, one place to start is rating and review websites, including ehrcompare.com, created by two optometrists, Adam Parker, OD, and Kevin Lafone, OD. You can also narrow the list of potential systems further by speaking with vendors and colleagues, visiting exhibit hall displays and trialing versions of their software to evaluate the functionality and ease of use.
Another important consideration is evaluating the list of instruments with which your desired EHR can integrate.
Create the Perfect Network
Once you have an EHR system in place, you’ll be able to interface with certain diagnostic instruments, whether they are existing instruments or those you acquire over time. Interfacing for tasks that are repeated frequently, such as lensometery and refraction, is a significant time-saver. An interfaced automated refraction system is particularly valuable because refraction is crucial to every comprehensive exam and requires a significant amount of data exchange. By comparison, while non-contact tonometers can also be interfaced with EHR, there is less value in doing so. IOP can be recorded with just one value per eye, while refraction has three values (sphere, cylinder and axis). With an integrated, automated refraction system, for example, the autolensometer measures the glasses prescription and then transfers the data to the EHR, automatically populating the sphere and cylinder values into the appropriate fields. If you have a complete automated refraction system—autolensometer, autorefractor, digital phoropter and digital visual acuity chart—all of the instruments can interface with each other and the EHR (Figure 1).
My new practice has a complete automated refraction system where the digital phoropter receives readings from both the autolensometer and the autorefractor. The lensometer, autorefraction and manifest refraction are all transferred from the digital phoropter, which acts as a hub, to the EHR through an instrument interface. Like many other optometrists, I have found this increases my efficiency by reducing the amount of time needed to record measurements, all while also eliminating transcription errors and significantly improving consistency.
“Arguably the most powerful use of efficiency with regards to EHR is to have your software integrated with an automated refraction system, along with the peripherals like an autorefractor/keratometer and automated lensmeter,” said Scott Shone, president of Ophthalmic Instruments, an independent dealer of ophthalmic instruments, in an interview. “To be able to test a patient with the autorefractor and autolensmeter in the pretest room, press a button and have that data transmitted to the automated refraction unit in the exam room is a tremendous time saver.”
Having such a set-up also allows the OD to “instantly compare the patient’s old Rx with their new prescription,” he says. Customized programs can include the full 21-point exam or any other refracting procedure you prefer. “The icing on the cake,”Mr. Shone says, is that once completed, the refraction, previous Rx, new Rx, automated reference data and so on can all be downloaded into the EHR program. “Not only does the information send over in a matter of seconds, but this eliminates any transcription errors as well.”
What Hurts Can Also HelpBecause most optometric practices still heavily rely on mercantile sales for revenue, it’s no surprise many optometrists are unhappy when patients fill their glasses and contact lens prescriptions elsewhere, including warehouse and online stores. But optometrists shouldn’t be so quick to shun these resource--s—they may offer other opportunities to save and promote efficiency. Many practice owners save time and money by purchasing their business supplies online and from warehouse stores. You can also tap into this third-party vendor system by hiring freelancers for graphic design, website and app development, digital marketing and on-hold telephone voice-overs, to name just a few. Most vendors have adapted to allow business owners to order or troubleshoot online, reducing time spent on hold waiting for service. While online patient ratings and reviews can strike a nerve with some clinicians, they can be invaluable when researching services that your business may need. |
Plan Your Space
The list of pre-exam measurements requires careful thought, as does the layout of diagnostic instruments. Ideally, the patient should not have to sit down and stand up multiple times. Because all of my patients undergo automated perimetry, autorefraction, fundus photography and retinal OCT, these instruments are all on the same instrument table, allowing sequential capture while the patient remains seated throughout the process. The autolensometer is placed on a fixed-height table since this does not need to raise or lower to accommodate the patient’s height. Automated perimetry is done before fundus photography so that the photographic flash does not cause an afterimage that can confound the visual field measurement. Meanwhile, my topographer is placed on its own instrument table because only certain patients require this measurement, thereby minimizing the burden on patients.
Admittedly, there is an advantage to building a new facility, since patient traffic flow can be streamlined, and electrical and cabling needs can be planned from the start, rather than retrofitting an existing space, which may pose more limitations. This is where a space planner that works within the eye care industry can be immensely helpful. They can produce drawings that will help you plan how to place your various instruments to maximize efficiency and patient flow (Figure 2).
For optometrists who have limited space within their practices, combination units are often a wonderful option. For example, my previous practice had a combined autorefractor, autokeratometer and a non-contact tonometer. This space saver was highly efficient for my prior workflow, especially considering it also integrated with the EHR.
Instrument distributors can be a valuable resource due to their familiarity with a cross section of instruments by different manufacturers, and they often know everything about each instrument’s speed and integration capabilities. Such knowledge can help you make the right choices when shopping for new equipment to integrate into your practice.
Secondary Interfaces
In the previous decade, many eye care EHR manufacturers concentrated their development efforts on allowing users to qualify for federal incentives. Unfortunately, many EHRs at the time lacked desirable functionality for communicating with patients and delivering desired practice metrics.
To provide these functions, a cottage industry of secondary software interfaces that transferred data out of the EHR databases into their software systems sprung up. Today’s patient communication software—customer relationship management systems—allow appointment reminders, exam recalls, surveying, marketing and so forth through e-mail, text and phone voice messaging. Other secondary platforms can help you gather practice management metrics, which can make a big difference when looking to implement data-driven business decisions. All these operations facilitate efficiency and reduce the burden on staff of having to pull charts and call patients.
More EHR companies are now developing their software to incorporate the functionality previously handled by these patient communication software and business dashboard systems—a welcome trend for practicing optometrists. For example, some EHRs now include patient portals that give patients the convenience of completing registration forms online before their appointment or upon arrival to the office using a workstation or tablet. The staff can then transfer the patient’s data directly into the electronic record. According to Carlos Rivero, regional account manager for My Vision Express (Insight Software), this “reduces the double data entry by the staff to enter demographic and health history information into the system.”
Many EHRs now also include patient communication modules that permit online patient scheduling and other patient communication functionalities, such as text and email appointment reminders, recall, optical status and birthday messages. Some may even include automated communication to patients who have not been in for an annual exam in the past 12 months and do not have active recall or an appointment scheduled in the system.
Call Them, and They Will ComeBy Kevin Henne, OD When adding technology to our practices, we’ve probably all been guilty of seeing nothing but another monthly payment, for which we will have to sell services and change our routines to recover the monthly expense. We always need to evaluate our practice patterns before a major purchase, but we also need to contemplate a host of other cost concerns, such as principal and interest, buying vs. leasing, property tax implications, Americans With Disabilities Act credit considerations, depreciation, service contract options, property taxes and longevity of both the instrument and the technology’s relevance. We can’t become bogged down by the paralysis of analysis—it’s one of the main reasons a practice can stagnate after 15 to 20 years. I was guilty of not investing in new technology at the rate I should have been because I thought I didn’t want to be paying off expensive equipment late in my career. But paying off expensive equipment is easier when you are excited about the improved care it provides. It’s also easier when you have a thriving, not withering, patient base. Upgrade and Explode In today’s high-tech practice, a patient communication software program is a must. In my own practice, finally investing in one caused a significant overnight jump in patient load. In my 35+ years in practice, this is the single greatest surprise—and the best thing I have ever done in practice. It is relatively inexpensive, and I believe you will recuperate the monthly subscription fee in the first two hours of each month that you use it. In addition, you can keep patients connected with your office without spending your staff’s valuable time. Keep the Ball Rolling This is why the patient communication system was the lynch-pin for my practice. Once I had the patient flow, I was able to delegate more of the actual data collection to my staff, giving me time to evaluate the data and ensure everyone was working to their highest level of training. It also has allowed me time to discuss examination findings with patients in greater detail and explore other topics related to their care such as contact lenses, nutritional supplements and ocular health such as glaucoma and cataracts. You can’t see patients if they don’t make appointments, and you can’t add services if you don’t have patients. It’s all connected. Adding technology can be the single most important improvement you make to your practice—as long as you add the right technology. For my practice, an improved communication tool made all the difference. |
A Team Approach
When technology is used properly, it can tackle repetitive tasks to reduce their burden. In optometric workflow, achieving high efficiency is a customized endeavor that requires careful implementation of the right EHR for your needs. From there, you must also coordinate diagnostic instruments and secondary software to interface with the EHR. The physical location of instruments, including cable drops and electrical outlets, plays an important role in overall efficiency as well.
All of this coordination doesn’t have to be on your shoulders, however; your instrument and EHR representatives, office space planner and IT professional all become an integral part of your office team, along with your clinical staff, to help you achieve the most efficient workflow and patient flow. n
Dr. Chou practices at ReVision Optometry in San Diego, where he directs a referral-based scleral lens and keratoconus clinic.
| 1. Mahdawi A. What jobs will still be around in 20 years? Read this to prepare your future. The Guardian. www.theguardian.com/us-news/2017/jun/26/jobs-future-automation-robots-skills-creative-health. June 26, 2017. Accessed July 25, 2018. |

