 |
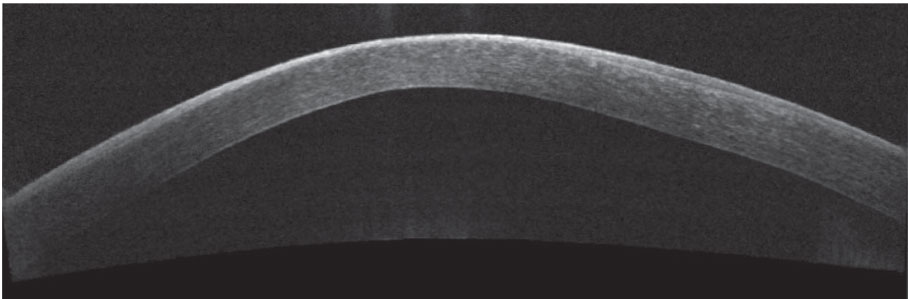
| Early intervention for keratoconus patients is crucial to optimize outcomes. Photo: Katelyn Lucas, OD. Click image to enlarge. |
The earlier keratoconus is recognized and treated, the better the outcome for the patient. A recent study’s survey findings support and confirm the necessity of collaborative management and prompt referral to save these patients’ sight.
“Eye problems are among the most common consultations in general practice, comprising approximately 5% of consults in the United Kingdom,” explained the researchers in their paper. “Some reports highlight that approximately half of patients with chronic eye diseases don’t receive regular eye care by an ophthalmologist.” One likely culprit: the lack of specificity that results from complaints of “reduced visual acuity” at time of presentation to the GP, which could point to any number of conditions, the authors suggest.
Keratoconus patients require management by a team of doctors that includes general practitioners, primary eye care providers, optometrists and ophthalmologists, the researchers said. However, the ideal state of this collaboration is unknown in Europe and elsewhere, including the US. The Portuguese Optometrist Association distributed an online survey via newsletters to assess keratoconus patient management and referral practice patterns among Portuguese practitioners. They received 119 responses and compared these with the responses of previously reported survey results of 464 eye care practitioners in the United Kingdom and Spain (n=126 and 338, respectively).
They found that most Portuguese respondents to the optometry survey had fewer than five new keratoconus patients each year (79% in Portugal, 71% in the UK, 76% in Spain). The researchers were unable to identify an accepted referral criterion because there was a good degree of variability. Only 14% of respondents in Portugal referred out at initial diagnosis, compared with 50% in the UK and Spain. A total of 32% referred out when they detected progression (vs. 17% in the UK and 30% in Spain), and 10% referred out when visual acuity was affected (vs. 9% in the UK and 6% in Spain). A large number of respondents (83%) in Portugal did not comanage with ophthalmologists (vs. 60% in the UK and 73% in Spain).
“Due to the prevalence and incidence of keratoconus, a relatively low number of new cases are expected to be detected by primary care practitioners, including general practitioners and primary eye care practitioners,” the researchers said. “However, it’s difficult to know if all keratoconus patients are detected early in primary eye care practice because the results of this study showed that a large number of eye care practitioners detected <5 new cases each year.”
“A delay in diagnosis increases the risk of vision loss or the need for a corneal transplant, and treatments such as crosslinking can help to halt progression, save patients’ vision and improve their quality of life,” they continued. “Unfortunately, a simple and cost-effective screening test isn’t currently available for the early diagnosis of keratoconus.”
Referral patterns in the UK, Spain and Portugal differ from those recommended by the American Academy of Ophthalmology (AAO). The AAO suggests avoiding referral whenever possible and waiting to refer until vision can’t be improved with spectacles or contact lenses, or when progression is confirmed. The researchers say the referral criteria they identified in the study “could cause a large number of patients to not receive appropriate treatment to halt keratoconus progression (such as crosslinking), which could result in a significant loss of vision. In fact, the Global Panel of Keratoconus and Ectatic Diseases recommends different management options to halt keratoconus disease in the early stages, including pharmacological and nonpharmacological treatments, to reduce the impact of keratoconus on patients’ quality of life.”
The researchers concluded that keratoconus patient care could be improved with early detection and referral to a specialist for a definitive diagnosis. They recommend using non-surgical management early, such as avoiding eye rubbing, anti-allergy treatment in atopic or allergy patients, preservative-free topical lubrication to reduce irritation, gas permeable contact lenses and crosslinking or other surgical options such as DALK. “These options require multidisciplinary collaboration,” they emphasized in their commentary.
Rahmani M, Ortiz-Toquero S, Martin R. Referral pattern and co-management of keratoconus patients in primary eye care: a survey of three European countries. Cont Lens Anterior Eye. November 10, 2021. [Epub ahead of print]. |

