Diabetes can cause irreversible and serious damage to the eyes, prompting researchers to look further into ways in which it may be identified earlier as a means of mitigating long-term consequences. One of these possibilities is use of a multifocal electroretinogram (mfERG), which objectively quantifies electrical activity in the retina and can be more sensitive to early changes than examination techniques alone.
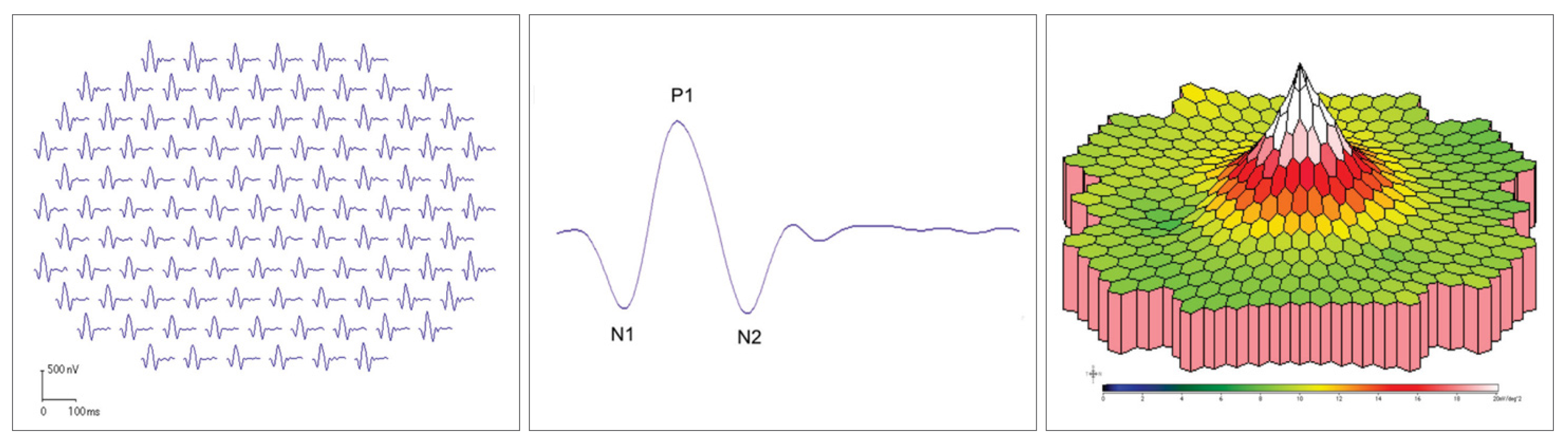 |
| mfERG results are presented as a series of waveforms indicating electrical activity in the retina at each stimulus point (left image) as well as a topographic map of the results (right image). A typical wave is shown in the middle figure. Photo: Hua Bi, OD, PhD. Click image to enlarge. |
In the test, a pattern of hexagonal stimuli are presented to the subject while electrodes measure electrical activity in the eye. Important terms include N1 (the negative phase), P1 (the positive phase), amplitude (maximum voltage recorded in response to stimuli) and implicit time (the amount of time it takes to reach maximum amplitude). The stimuli are organized in a series of concentric rings, typically five in all, and results of each can be analyzed individually.
In a new study, researchers in Bejing recently evaluated changes of retinal function in type 2 diabetes patients without apparent diabetic retinopathy using mfERG. Included were 36 DM patients (72 eyes) comprising the experimental group and 35 individuals (70 eyes) in the control group. After mfERG analysis of both groups, the study researchers were able to determine a significant delay in implicit time of the P1 wave in the first, third, fourth and fifth rings of the experimental group. The implicit time of the N1 wave was also delayed compared to the control group in the fourth and fifth rings. The experimental group saw implicit time of the P1 and N1 waves in the temporal region being delayed; however, there was no observed difference between the groups of the temporal area in the amplitude density of the P1 and N1 waves. As well, no difference was seen in implicit time and amplitude density of the N1 and P1 waves in the nasal region between groups.
|
To learn more about uses of electrodiagnostic testing in optometric practice, see this recent article by Bisant Labib, OD. |
In their paper on the study, the researchers note that the mfERG complex parameters showed better specificity and sensitivity in the diagnosis of diabetic retinopathy, thus prompting them to relay that “the mfERG complex parameter is a potential indicator for the early diagnosis of diabetic retinopathy.”
Elaborating on their findings, the authors point out that there are debatable points on amplitude change. Some studies have concluded mfERG’s first- and second-order amplitude responses increase in DR. In this study, though, the P1 wave amplitude density of the first to fifth ring was lower than controls, but without statistical difference.
As for the delay, they found of implicit time for both P1 and N1 waves in some areas of the retina, the authors explain this potentially being caused by capillary network occlusion in the inner nuclear layer at early stage diabetes, leading to ischemia, hypoxia and an undetectable non-perfusion area.
Finally, they discuss that previous research has found decreased, uneven retinal distribution of implicit time delays in those with no diabetic retinopathy vs. those with nonproliferative retinopathy. In that study, abnormalities were more common in the inferior retina, likely because of greater ischemic susceptibility. The current study found greater sensitivity to hyperglycemic injury of the temporal rather than nasal region. A possible explanation for this is due to temporal retinal vessels having poor expansion reserve capacity under ischemic and hypoxic conditions, thus more intolerant to hypoxia.
The researchers summarize their findings by stating that, “in general, the function of the retina has been abnormal for a significant period before diabetes patients have visual retinopathy.” Clinically, this indicates that “mfERG can more sensitively reflect the abnormality of retinal function and can be used to evaluate the retinal function of early diabetes patients without visible retinopathy.”
Li RR, Yang Y, Zhang MG, et al. Abnormalities of retinal function in type 2 diabetes mellitus patients without clinical diabetic retinopathy detected by multifocal electroretinogram. BMC Ophthalmol. 2024;24(1):71. |

