 |
Q: I have a patient with marked vascularization and progressive lipid keratopathy (LK) in one eye. What treatment options are available today?
A: LK is a progressive disease characterized by an accumulation of fat deposits with adjacent abnormal vascularization in the cornea,” says Larae Zimprich, OD, of Vance Thompson Vision. “This condition, whether idiopathic or secondary to corneal or systemic disease, typically opacifies and can interfere with visual acuity.”
Dr. Zimprich notes that LK treatment aims to prevent new blood vessel formation. Current options include corticosteroids, photodynamic therapy (PDT), anti-VEGF antibodies, argon laser treatment, needlepoint cautery and penetrating keratoplasty (PKP).1
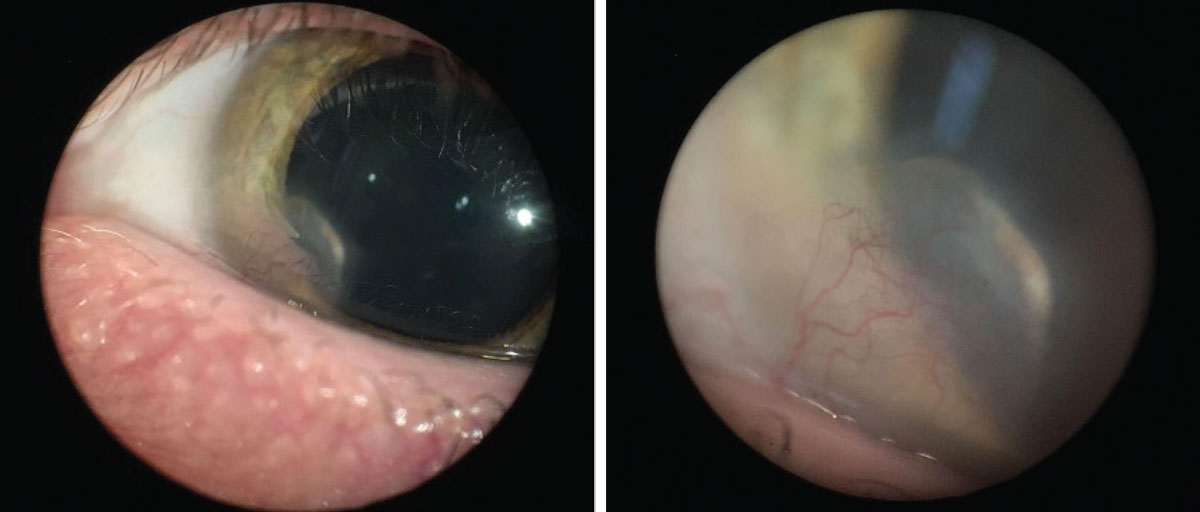 |
| Fat deposits with adjacent abnormal vascularization in the cornea are characteristic of LK. Click image to enlarge. |
Ophthalmic Options
Topical corticosteroids are commonly used due to their anti-inflammatory properties.1 However, Dr. Zimprich notes that neovascularization can form in the absence of inflammation; therefore, if the etiology is not inflammatory, then corticosteroids will not be effective. She adds that prolonged steroid use also has well-known side effects, including increased risk of developing cataracts and glaucoma. Due to these reasons, there may be better treatment alternatives.
PDT, first introduced to ophthalmology in 2000, uses a vascular-selective, light-sensitive substance, such as verteporfin or dihematoporphyrin, in combination with a low-power infrared laser.2 It is commonly used to treat vascular issues in the retina and choroid.
While treating LK, verteporfin or dihematoporphyrin is injected into the cornea, leading to endothelial damage, microvascular thrombosis and blood vessel occlusion.1 This therapy can be repeated if needed, although Dr. Zimprich says one major disadvantage is the higher cost to patients.
Administration of anti-VEGF antibodies, such as bevacizumab and ranibizumab, through topical, subconjunctival or intracorneal injections has also proven to be effective, according to Dr. Zimprich. VEGF is a key mediator in angiogenesis; therefore, these antibodies block new VEGF-mediated vessel formation, she adds.
Multiple studies have shown that VEGF increases vessel permeability, which could account for lipid leakage and LK development.1 When used as topical medication, 1.0% ranibizumab QID for three weeks proved to be slightly more effective than 1.0% bevacizumab with the same drop regimen in reducing neovascularization.3 Otherwise, use of subconjunctival and intrastromal injections of bevacizumab can regress deep neovascularization.1
Argon laser treatment works to occlude pathologic vessels by directing a beam of light and utilizing heat energy.1 Dr. Zimprich says that laser-induced tissue destruction can cause more harm than good in some cases, with worse neovascularization due to the intense inflammatory response and potential subsequent hemorrhaging, corneal thinning and iris atrophy.
Another treatment option is electrolysis needle cauterization, which uses direct thermal cautery to target the small, fine vessels.1 The cauterization may have to be repeated multiple times to reduce the neovascularization and lipid deposits, Dr. Zimprich notes. When other therapies cannot achieve desirable results, a PKP may be indicated.1 The prognosis may be guarded in severe cases with dense neovascularization, as the risk of rejection increases in these circumstances, she adds.
Future Outlook
All of the previously discussed treatment modalities have proven effective against LK, with newer management options on the horizon.
One promising up-and-coming development, currently in its early stages of research, is mitomycin intravascular chemoembolization (MICE).1 This procedure consists of intra-arterial infusion of mitomycin-C with an artificial embolus to cause vessel occlusion. Successful occlusion could eliminate or prevent LK in early stages of the disease. Unfortunately, MICE is somewhat time-consuming, as it can be difficult to target afferent vessels, and infusing efferent vessels can worsen LK.1 Studies are currently in progress to determine proper technique, efficacy and safety.
Luckily, what’s available today gives practitioners plenty of viable options and offers patients the chance to experience successful visual outcomes. Stay up-to-date and informed on the latest LK treatment offerings to provide the best care to this demographic.
Dr. Shovlin, a senior optometrist at Northeastern Eye Institute in Scranton, PA, is a fellow and past president of the American Academy of Optometry and a clinical editor of Review of Optometry and Review of Cornea & Contact Lenses. He consults for Kala, Aerie, AbbVie, Novartis, Hubble and Bausch + Lomb and is on the medical advisory panel for Lentechs.
1. Hall MN, Moshirfar M, Amin-Javaheri A, et al. Lipid keratopathy: a review of pathophysiology, differential diagnosis, and management. Ophthalmol Ther. 2020;9(4):833-52. |

