The hazards that accompany high myopia are well known by now, but studies have not adequately documented the long-term peripapillary changes on OCT in adult myopia before. Researchers in Shanghai recently provided such an evaluation using enhanced-depth imaging SD-OCT. Their multivariate analysis demonstrated a strong association between changes in axial length (AL) and peripapillary microstructures, including border tissue length, Bruch’s membrane opening diameter and peripapillary anterior sclera angle in adult myopic eyes.
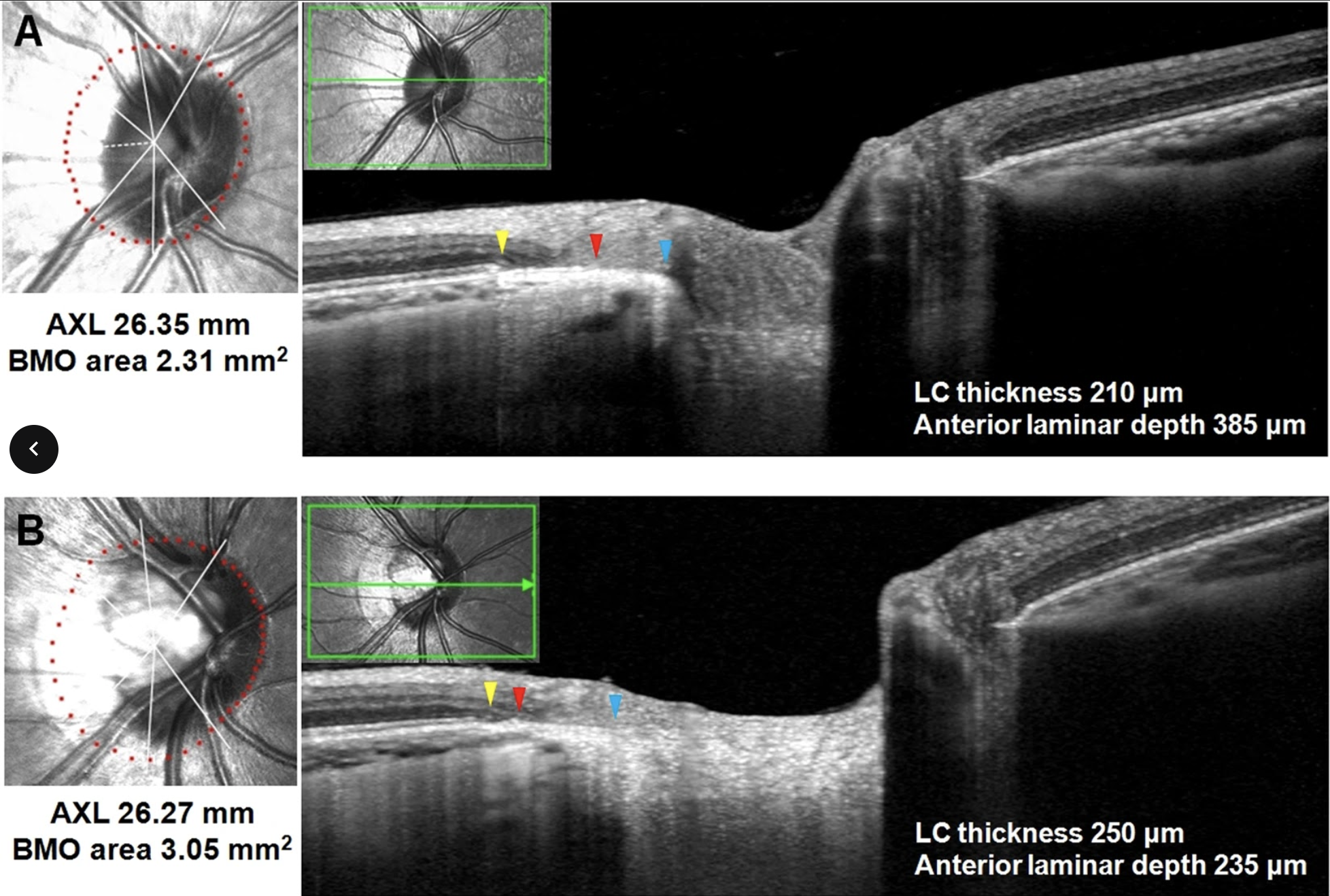 |
| A marked change of peripapillary structures, including border tissue, Bruch’s membrane, choroid and sclera, could be observed not only in adult eyes with high myopia but also in those with moderate myopia to a lesser extent. These images, from a different study, show myopic eyes with similar axial length but different presentations of peripapillary changes indicative of high myopia. Photo: Sung, MS, et al. Sci Rep 10, 4607 (2020). Click image to enlarge. |
The study included 65 eyes of 33 participants with a minimum eight-year follow-up (mean: 9.46 years). The mean age was 36.8 years (range: 22 to 67), and the mean axial length was 25.7mm at the initial visits. Based on the final axial length, eyes were classified as mild myopia (AL under 24.5mm), moderate myopia (AL from 24.5mm to just under 26.5mm) and high myopia group (AL of 26.5mm or higher). Enhanced-depth imaging scans (Spectralis, Heidelberg) were performed around the optic disc in the follow-up mode, which enabled capturing of the same positions.
The major finding of this study was that the optic nerve head (ONH) in adult myopic eyes may continue to change, not only in highly myopic eyes but also in moderate myopic eyes to a lesser extent. The border tissue, peripapillary Bruch’s membrane, choroid and sclera all underwent characteristic changes after nearly 10 years, with axial length showing an annual increase of 0.057mm in the high myopia group and 0.015mm in the moderate myopia group. At the last visit, the average border tissue length and Bruch’s membrane opening diameter were increased.
The development of Bruch’s membrane defect and inward protrusion of sclera on temporal peripapillary region was observed on eight (34.8%) eyes in the high myopia group, along with an extreme thinning or disappearing of peripapillary choroid. The change of border tissue length was significantly different in three subgroups, and the most marked elongation (20%) was seen in the high myopia group. Compared with other parameters, border tissue exhibited the most pronounced increase in this study. Taken together, the researchers suggested that border tissue appears to be a sensitive microstructural marker reflecting the progression of myopic optic disc for both children and adults.
“Our findings further suggest that the similarities and differences in the mechanisms of scleral degeneration during the process of axial elongation in high myopia and the aging deserve an in-depth study,” the study authors wrote in their paper, which was published in American Journal of Ophthalmology. “The current study indicated that the tension due to scleral protrusion and choroidal atrophy may lead to the rupture of peripapillary Bruch’s membrane during the long course of axial elongation in high myopia.”
“Such changes may impact the biomechanical environment around ONH and provide clues to the relationship among myopia, aging and glaucoma,” they concluded.
Dai Y, Wang L, Hong J, Sun X. Eight years and beyond longitudinal changes of peripapillary structures on oct in adult myopia. Am J Ophthalmol. March 21, 2024. [Epub ahead of print]. |

