Six weeks after the first confirmed case of SARS-CoV-2 (COVID-19) appeared at a large practice in New York City, it has become clear that the virus has changed medicine as we know it. At the outset, it was quickly apparent that integrating telemedicine into our daily practice was essential.
As optometrists in a large academic ophthalmology practice, we used creativity and innovation to make meaningful contributions during these unprecedented times. We learned that our best opportunity to do this was to staff the frontlines of triage and embrace telemedicine. To achieve this, we had to tackle several hurdles, including choosing appropriate software, understanding proper documentation and instituting new communication techniques with patients. Additionally, implementation required constant self-reflection and feedback, both from patients and colleagues, to determine what works and what doesn’t.
We now have 300+ triage calls and 200+ telemedicine visits for emergency eye care under our belt at a large practice in New York City, the epicenter of COVID-19. We have learned vital lessons: consent is key, prepare the patient, protect your privacy, consolidate your telemedicine resources, standardize documentation templates, arrange your emergency consult team and focus on follow up and patient tracking. While we continuously adapt, innovate and improve our telemedicine process, we still don’t know what the future holds.
Now, the next phase is expanding in-person visits. We have spent many hours on developing policies and protocols that prioritize patient protection and provider safety. Here, we outline a roadmap as our department plans to re-open our practice over the next several months.
(Ed. note: the advice provided here is from anecdotal sources and may not conform to state or federal guidance. Use your own discretion whenever contemplating changes to clinical or business practices.)
Step 1: Construct Patient Categories Based on The Level of Urgency
We started with categories A, B and C (Table 1). Category A patients are known emergencies or require an in-office visit due to the critical nature of their current condition. After category A, how you decide to rank you patients will matter on your practice type and area of expertise. For us, the gray area between A and B includes more urgent, but not emergent, patients. Category B patients have chronic conditions that merit quarterly monitoring. Category B-C includes those who commonly require follow-up every four to six months, but could be pushed out further. Finally, category C patients are the yearly routine exams.
Identifying which patient belongs to which category can be daunting, but it will allow you to properly triage the urgency of your patients’ needs. Assign a technician or staff member who knows your patients well to assign patients to each of the categories. Additionally, every patient who calls in with a problem and goes through triage should be classified into a category.
.jpg) |
| Click table to enlarge. |
Step 2: Map out the Next Three to Six Months
Uncertainty is the best word to describe this entire situation, and even the timeline for reopening, depending on state recommendations. Your best course of action is to plan the next three to six months and identify an appropriate time range for patients in each category.
Step 3: Optimize Your Office Space and Patient Schedule
Every office layout is unique; however, the concept of social distancing is crucial everywhere. Start by taking a look at the available space and locations and decide how many providers can be functioning at the same time. In a solo practitioner practice, this might only require decreasing patient numbers.
In a multiple doctor practice, MD/OD, academic or hospital setting, this step will take more planning. Ideally, no two practitioners would be occupying the same hallway. This limits the staff-patient interaction and patient-to-patient contact. Waiting rooms, dilating areas and testing spaces all need reconfigured to ensure proper distancing.
Physician schedules are now spaced out so no two patients need the same space at the same time, while also allowing staff time to take all infection precautions.
In addition, the tests you perform will likely change. For example, we are delaying visual fields during the pandemic.
 |
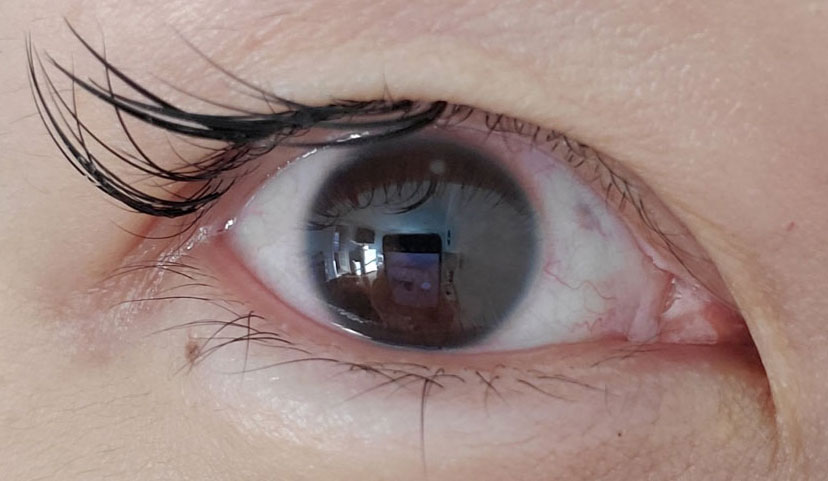 |
| Dr. Sherman uses telemedicine to help these patients with preseptal cellulitis, above, and a corneal infiltrate due to overnight contact lens wear, below. Click image to enlarge. |
Step 4: Reduce In-office Chair Time and Exposure
The increase in telemedicine technology and the unprecedented, albeit temporary, lift on HIPAA restrictions allows us to combine our in-office visits and telemedicine.
The concept of a diagnostic day could play a large role in your office. The patient could come in for their diagnostics, spend a limited amount of time with you in the exam room and then receive a phone call or audiovisual visit the next day to discuss results and next steps.
Innovative ideas and techniques on how to collect data on the patient, while also reducing face-to-face chair time, will be key as we merge our telemedicine practice and in-person visits.
Step 5: Plan to Implement Telemedicine in Standard Office Care
Triage telemedicine will still be essential as we transition back to practice. Due to social distancing and space constrictions, not all doctors will be able to practice in the office fives days a week. This is where telemedicine comes into play—it’s here to stay, and we must consider how to apply it into our practices long-term.
Patient and staff safety remain the top priority in any healthcare setting during the COVID pandemic. To keep everyone safe, optometrists must remain open to change.
We are looking forward to the next phases of patient care, regardless of what it will look like—whether in person, online or a combination of both.
Dr. Sherman is an assistant professor of optometric sciences and director of optometric services in the Department of Ophthalmology at Columbia University Irving Medical Center (CUIMC).
Dr. Kresch is a clinical instructor of optometric sciences in the Department of Ophthalmology at CUIMC.
Dr. Amaro-Quireza is a clinical instructor of optometric sciences in the Department of Ophthalmology at CUIMC.

