 |
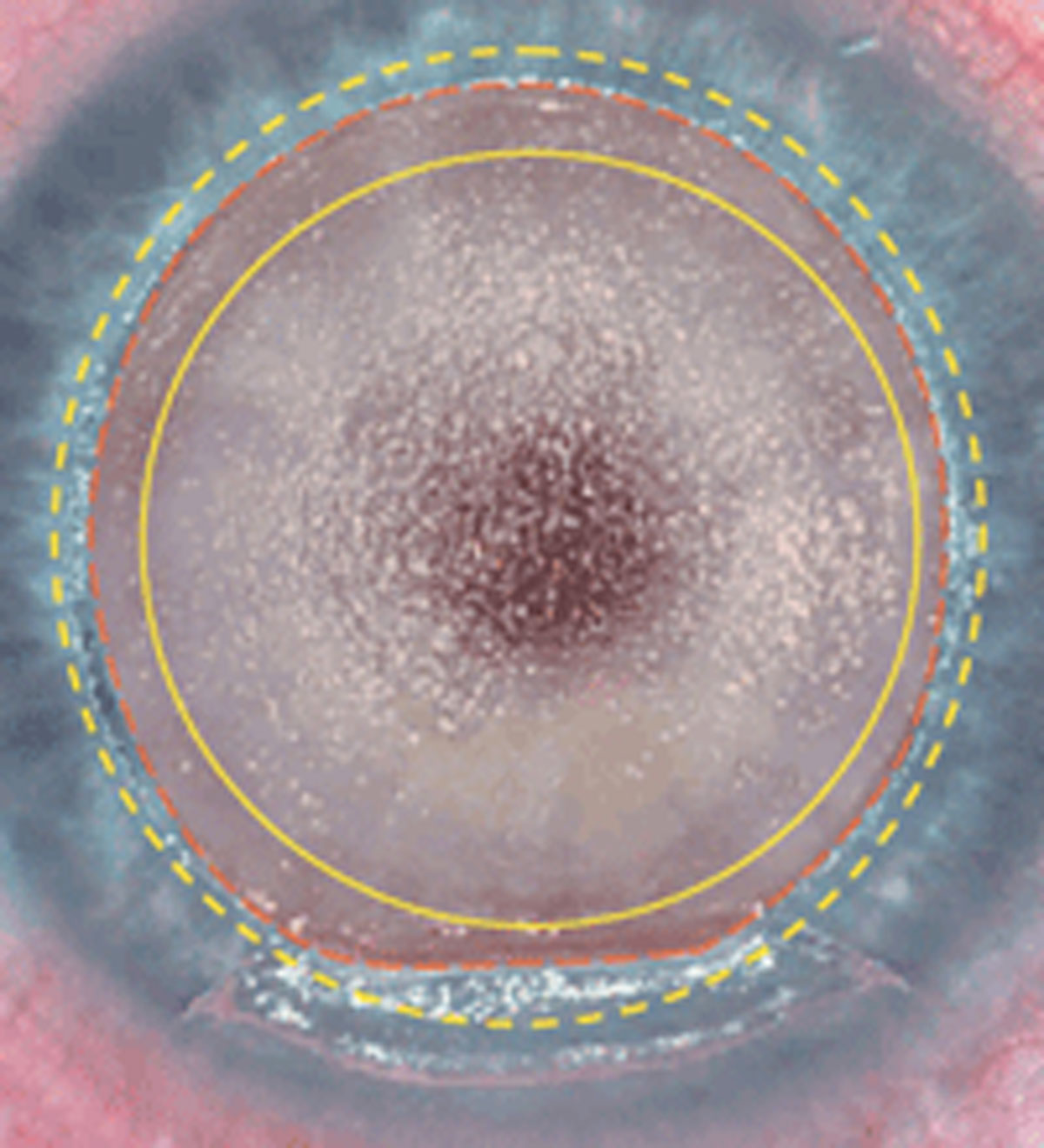
| Transepithelial PRK and LASIK may both be better options following keratoplasty, as conventional PTK can demonstrate the complication of haze. Photo: Martin L. Fox, MD. Click image to enlarge. |
Ametropia after keratoplasty can severely limit patients’ visual acuity. Frequently seen are cases of irregular astigmatism, typically linked with high degree myopia or hyperopia. A recent systematic review appearing in Journal of Cataract and Refractive Surgery investigated how safe and effective laser refractive surgery really is for patients who have previously undergone corneal transplantation.
Including a total of 31 studies, 732 eyes of 683 participants were evaluated, with refractive errors ranging from moderate hyperopia to high myopia with both regular and irregular astigmatism. The study researchers found that mean astigmatism and mean spherical equivalent improved significantly between the pre- and post-op periods, with 50% exhibiting the 1.0D range of target refraction. Of 586 patients, 5.8% lost two or more lines of corrected distance visual acuity after refractive treatment. Eyes with 20/40 uncorrected visual acuity or better was reported to be 46.8%.
Overall, laser refractive procedures, including LASIK, PRK and transepithelial PRK (T-PRK) were regarded as relatively safe and effective, with improvement in all outcomes. The only main adverse outcomes were haze from PRK and epithelial ingrowth from LASIK, which the authors point out are issues that arise even in virgin eyes. Even better, the potential complication of increased graft rate rejection was not determined when compared with other studies, sitting at 2.1%.
LASIK and PRK outcomes were comparable, with PRK notably demonstrating a higher concern in terms of haze development after procedure. T-PRK, however, is considered simpler and safter than PRK and has not seen any cases develop significant haze, as one prior study investigated. Astigmatic keratotomy is most commonly used for refractive surgery for astigmatism following keratoplasty, but this procedure is more unpredictable, and patients often need subsequent procedures to get to the level of significant visual improvement, since this keratotomy only offers cylindrical correction.
Some patients have had different refractive procedures before laser treatment, ranging from reasons of unsatisfactory results, pre-planned corneal irregularity reduction and high refractive errors. The authors point to techniques in refractive surgeries that may help, like using a two-step technique in LASIK. Creation of a lamellar flap by itself, followed by laser ablation on two different accounts, is proposed to be more predictable than a one-step version. One study first used surface ablation to regularize the cornea, with a second ablation to correct refraction error.
Two studies included in the meta-analysis used OCT, one to measure corneal thickness, and the other to evaluate the graft. These findings were not applicable to any correlation of differences in results among technique type. Further expanded upon, most studies only had one arm of intervention with heterogeneity between procedures, while heterogeneity also stemmed from etiology for performing keratoplasty and pretreatment regularity status of the cornea’s surface.
In general, the authors found that studies with longer follow-up duration saw stable refractive results with only minor visual regression, which could be explained by other conditions. In the future, the authors would suggest that “research could investigate the use of vectorial analysis in post-keratoplasty eyes, with consideration for the irregular astigmatism that can occur after this procedure. This could help to better understand the impact of surgically induced astigmatism on visual outcomes in this population.”
Alsubhi AH, Alhindi N, Abukhudair A, et al. Safety and efficacy of laser refractive procedure in eyes with previous keratoplasty—a systematic review and meta-analysis. J Cataract Refract Surg. 2023. [Epub ahead of print]. |

