 |
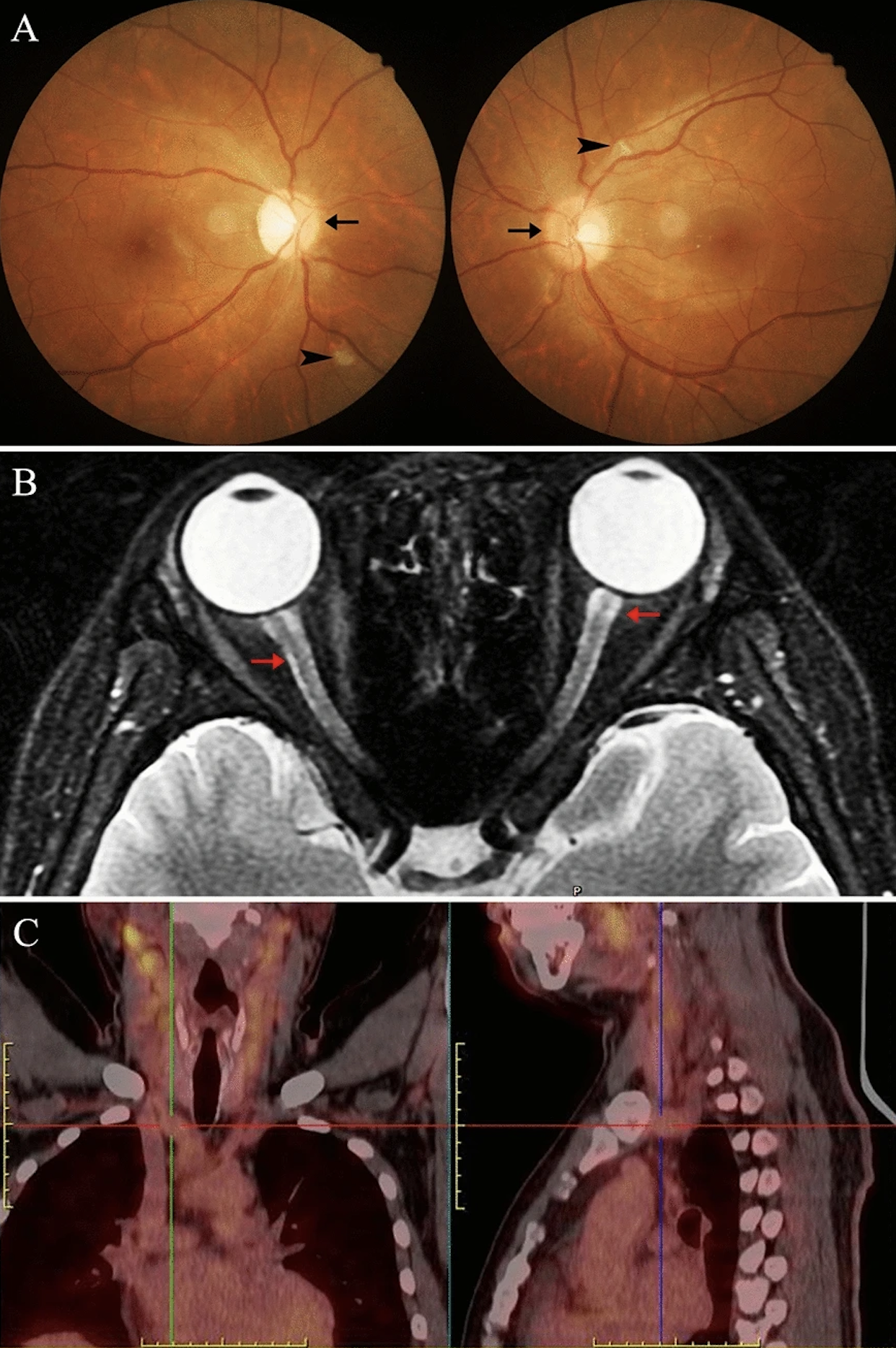
| Optic nerve involvement is reportedly 0.8% in granulomatosis with polyangiitis and 8% in microscopic polyangiitis patients. These images from the study show a case of a 32-year-old man with (A) bilateral disc edema and cotton wool spots; (B) discrete T2-weighed hyperintense signal at both the optic nerve and sneath (red arrow); and (C) evidence on PET imaging of multivessel disease through high accumulations of radioisotopes. Photo: Tang S, et al. Int Ophthalmol. 2024;44:387. Click image to enlarge. |
While vasculitis only rarely affects the eye, by means of the optic nerve, it can lead to irreversible visual damage when it does occur, causing vesicular inflammation and arterial, vein and capillary bed necrosis. Due to its serious nature, researchers in Beijing wanted to investigate clinical and imaging characteristics of PSV-associated optic neuritis cases. Their study was recently published in International Ophthalmology.
The retrospective investigation included 14 patients (21 eyes) who all received orbital MRI scans; enrolled were 10 men and four women, with ages ranging from 30 to 86 years. MRI of the orbits can detect if there is enlargement and/or enhancement of the optic nerve. Cases one through five reported a confirmed diagnosis of Takayasu’s arteritis, cases six through eight had giant cell arteritis and cases nine through 13 were antineutrophil cytoplasmic antibody–associated vasculitis. Case 14 was Cogan’s syndrome.
Interestingly, in all 14 cases, disease onset was during the fall or winter, and multiple organs and tissues were affected, including the kidneys, heart, paranasal sinuses, meninges and respiratory system.
In the discussion section of their paper, the authors further explain how PSV manifests ocularly. Retinal vasculitis characteristically displays tortuosity and dilation of retinal vessels or occlusion of the retinal artery; in most PSV-optic neuritis cases, localized occlusions of the retinal artery were seen in the acute phase which converted eventually to atrophy of a sector at later stage. Giant cell arteritis-associated small artery end inflammation commonly leads to arteritic anterior ischemic optic neuropathy, and Takayasu’s arteritis-associated hypertension or carotid occlusion frequently induces ocular ischemic syndromes and retinopathies. As such, ocular involvement does not seem to be caused by vasculitis directly.
What’s more, anterior segment manifestations are more prominently noticed in antineutrophil cytoplasmic antibody-associated vasculitis, according to previous research. Cogan’s syndrome is typically characterized by recurring episodes of deafness and visual loss from cochleovestibular dysfunction and interstitial keratitis, respectively; however, atypically, they can present with uveitis (37%), scleritis (23%), conjunctivitis (10%), cataract and other ocular manifestations.
With these facts in mind, the authors of the study suggest in their paper that “the autoantibodies’ attack on the optic nerve, ischemic damage or destruction of the blood-brain barrier may be the potential pathogenesis of vasculitis-associated optic neuritis. Even with prompt and aggressive clinical interventions, the prognosis remains unsatisfactory.”
They further stress that “PSV-optic neuritis is a fatal disorder as it can lead to acute visual or central visual field loss. PSV is a critical pathogenesis for the onset of optic neuritis, although it is rarely reported. Diagnosis of PSV-optic neuritis may sometimes be delayed or misinterpreted in complex clinical manifestations of vasculitis,” and that “an early diagnosis is crucial for preventing irreversible injuries to the optic nerve.”
| Click here for journal source. |
Tang S, Zhou H, Li R, et al. The primary systemic vasculitis associated optic neuritis: a retrospective analysis in a single center over 10 years. Int Ophthalmol. 2024;44:387. |

