 |
Q: I have a graft patient with advanced glaucoma who needs a scleral lens. Should I be concerned about an increase in IOP? If so, what are my other options?
A: The relationship between scleral lens wear and IOP is well documented through a multitude of studies, according to Langis Michaud, OD, professor at the University of Montreal.
Research Findings
A 2016 study hypothesized that sclerals can contribute to increased IOP through compression of the episcleral veins and/or Schlemm’s canal.1 This implies that IOP is restored as soon as the lens is removed or the compression is released.
One review reported a 5mm Hg to 30mm Hg increase in IOP following one hour of glass scleral use.2 Another established that glaucoma patients experience a pressure spike upon scleral lens removal and a longer recovery time.3
One report found no IOP variation at lens removal as measured by air tonometer.4 Another used a pneumotonometer during lens wear (one to two hours) and observed high inter-subject variability, but little increase on average.5 With a Tonopen (Reichert), researchers found a <1mm Hg increase in IOP after PROSE lens wear.6
A rebound tonometer resulted in a 5mm Hg gain (one patient spiked 15mm Hg) after eight hours of lens wear.7 These results match another recent study that used a Diaton transpalpebral tonometer (Escalon Medical) during four hours of lens wear and documented an IOP increase of 5mm Hg regardless of the lens diameter.8
A study applying Goldmann tonometry through a fenestrated scleral found IOP increase of 4mm Hg in the minutes following lens application.9 Another found no variation using a Schiotz tonometer (Medline) applied on the conjunctiva during four hours of wear.10
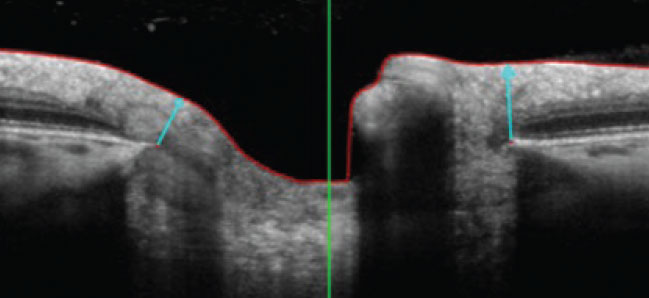
The most interesting studies are coming from optic nerve head observation during lens wear, says Dr. Michaud. One found minimum rim width (MRW) thinning during six hours of scleral lens wear, which objectively translates into an IOP increase.11 Another study also looked at MRW but took into account diurnal physiological variation as well.12 The team found that IOP increased significantly (average 5mm Hg) over six hours of lens wear.12
 |
|
Arrows illustrate the MRW assessment. Click image to enlarge. |
Clinical Takeaways
Due to conflicting and inconsistent findings, no formal conclusion regarding scleral lens wear and IOP changes can be made at this point, notes Dr. Michaud. Nonetheless, these elements must be considered:
- Solid trends prove that IOP can rise during scleral lens wear (range of 0mm Hg to 30mm Hg with an average of 5mm Hg over four to six hours of use).
- High inter-subject variability means we cannot predict who will spike and who will remain stable.
- Keratoconus may also occur, as there is a higher prevalence of normotensive glaucoma in this patient population.13
- Lens design/diameter likely does not influence the outcome. Most lenses land around the same area, and the lens weight is not distributed along the conjunctiva with a larger scleral lens.
- Longitudinal studies are needed to evaluate IOP in different populations.
- Scleral lenses are not likely to induce glaucoma in a normal patient. But close monitoring is recommended.
Knowing this information, remain very cautious when caring for severe glaucoma patients, warns Dr. Michaud. He suggests exploring other ways to compensate for corneal irregularities and restore visual acuity before considering scleral lenses, including hybrid and gas permeable lenses.
If scleral lenses are fitted as a last resort, Dr. Michaud recommends limiting lens compression through toric and flatter peripheral curves, fenestrations, channels, etc. He adds to pay close attention to the optic nerve profile and visual fields. As a final thought, he emphasizes that IOP measurement at lens removal is not indicative of what is happening during wear.
Dr. Shovlin, a senior optometrist at Northeastern Eye Institute in Scranton, PA, is a fellow and past president of the American Academy of Optometry and a clinical editor of Review of Optometry and Review of Cornea & Contact Lenses. He consults for Kala, Aerie, AbbVie, Novartis, Hubble and Bausch + Lomb and is on the medical advisory panel for Lentechs.
1. McMonnies CW. A hypothesis that scleral contact lenses could elevate intraocular pressure. Clin Exp Optom. 2016;99(6):594-6. 2. Hugert A. Increase of the intraocular pressure when using contact glasses. Acta Ophthalmol. 1951;29(4):475-81. 3. Huggert A. The intraocular pressure in glaucomatous eyes, following the use of contact lenses. Acta Ophthalmol (Copenh). 1953;31(2):141-52. 4. Vincent SJ, Alonso-Caneiro D, Collins MJ. Evidence on scleral contact lenses and intraocular pressure. Clin Exp Optom. 2017;100(1):87-8. 5. Nau CB, Schornack MM, McLaren JW, et al. Intraocular pressure after 2 hours of small-diameter scleral lens wear. Eye Contact Lens. 2016;42(6):350-3. 6. Shahnazi KC, Isozaki VL, Chiu GB. Effect of scleral lens wear on central corneal thickness and intraocular pressure in patients with ocular surface disease. Eye Contact Lens. 2020;46(6):341-7. 7. Aitsebaomo AP, Wong-Powell J, Miller W, et al. Influence of scleral lens on intraocular pressure. JCLRS. April 22, 2019. [Epub ahead of print]. 8. Michaud L, Samaha D, Giasson CJ. Intra-ocular pressure variation associated with the wear of scleral lenses of different diameters. Cont Lens Anterior Eye. 2019;42(1):104-10. 9. Cheung SY, Collins MJ, Vincent SJ. The impact of short-term fenestrated scleral lens wear on intraocular pressure. Cont Lens Anterior Eye. 2020;43(6):585-8. 10. Obinwanne CJ, Echendu DC, Agbonlahor O, et al. Changes in scleral tonometry and anterior chamber angle after short-term scleral lens wear. Optom Vis Sci. 2020;97(9):720-5. 11. Walker MK, Pardon LP, Redfern R, et al. IOP and optic nerve head morphology during scleral lens wear. Optom Vis Sci. 2020;97(9):661-8. 12. Samaha D, Michaud L. Bruch membrane opening minimum rim width changes during scleral lens wear. Eye Contact Lens. 2021;47(5):295-300. 13. Cohen EJ, Myers JS. Keratoconus and normal-tension glaucoma: a study of the possible association with abnormal biomechanical properties as measured by corneal hysteresis. Cornea. 2010;29(9):955-70. |

