 |
Q:
I have an 18-year-old keratoconus (KC) patient with progressive disease on topography and acuity reduction who appears to be a good candidate for corneal crosslinking (CXL). However, he had a bad adenoviral infection about nine months ago and still has residual subepithelial infiltrates (SEIs) that he is taking topical cyclosporine for. When would it be safe to do CXL, if ever?
A:
The patient’s SEIs may confound a clinician’s ability to isolate the underlying cause(s) of acuity reduction and topographic progression, according to Clark Chang, OD, director of cornea specialty lenses at Wills Eye Hospital and director of clinical services at TLC Vision. Further complicating things, Dr. Chang notes that, although ultraviolet (UV) light irradiation has antimicrobial and antifungal therapeutic properties, it is not yet known how UV emissions during CXL affect viral residence within the cornea. These clinical factors make it difficult to determine CXL candidacy and treatment timing for this patient.
Next Steps
Dr. Chang says the conservative management approach would be to provide additional topical therapies to aggressively reduce or eliminate the SEIs prior to CXL treatment. He suggests adding topical corticosteroids to the current topical regimen of cyclosporine and says it may be worth increasing the dosing frequency of either topical medication, or both, in the short term to attempt to obtain quicker clinical control on the inflammatory activities within the cornea.
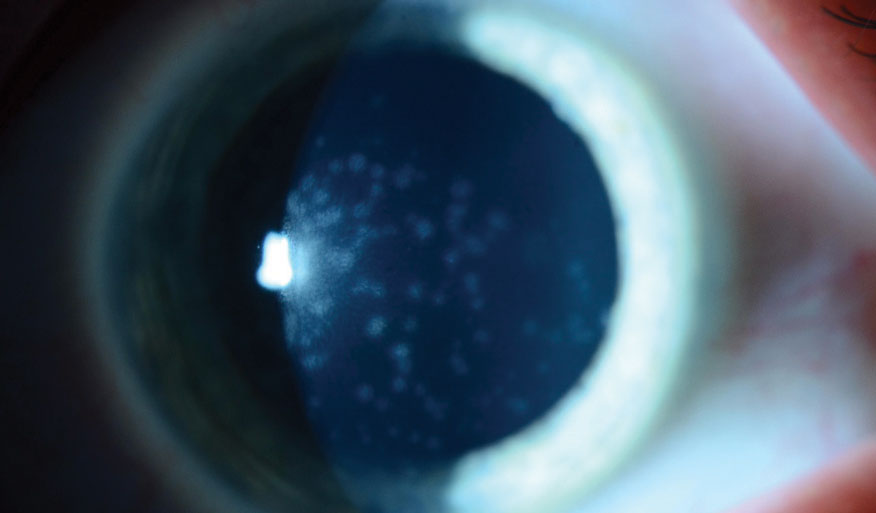 |
| This patient has persistent SEIs. Photo: Christopher Rapuano, MD. Click image to enlarge. |
Progressing with Progression
KC management, however, must maximally protect patients from potentially preventable loss of function. Dr. Chang notes that the decision to provide CXL to a KC patient does not always require documented disease progression. However, given the presence of SEIs that could complicate treatment, he says it is wise to first obtain definitive documentation.
If SEIs are deemed quiescent by the clinician, Dr. Chang says they presumably will not interfere with tomographical tests. Thus, he recommends documenting any corneal changes in posterior corneal elevation profile, posterior corneal curvature and pachymetric distribution.
Due to the patient’s young age, Dr. Chang says he’ll have a higher risk for KC progression over his lifetime. So, despite the presence of SEIs, if KC progression is detected, even if it is only mild, he notes that providing CXL treatment may be justified given the deterioration in visual function. Before proceeding with CXL under these circumstances, however, Dr. Chang suggests providing education on the off-label use of CXL and the post-op risk of exacerbated SEIs.
If the patient and his parents have concerns and decide against immediate CXL treatment, Dr. Chang recommends continuing the previously discussed topical therapies and monitoring the cornea every one to two months. This, he adds, will increase the chances of detecting KC progression at a future time point, which would increase the medical necessity of CXL treatment. If CXL is performed, Dr. Chang suggests stressing the importance of avoiding eye rubbing before and after treatment and keeping the patient on a slower post-op topical steroid taper.

