 |
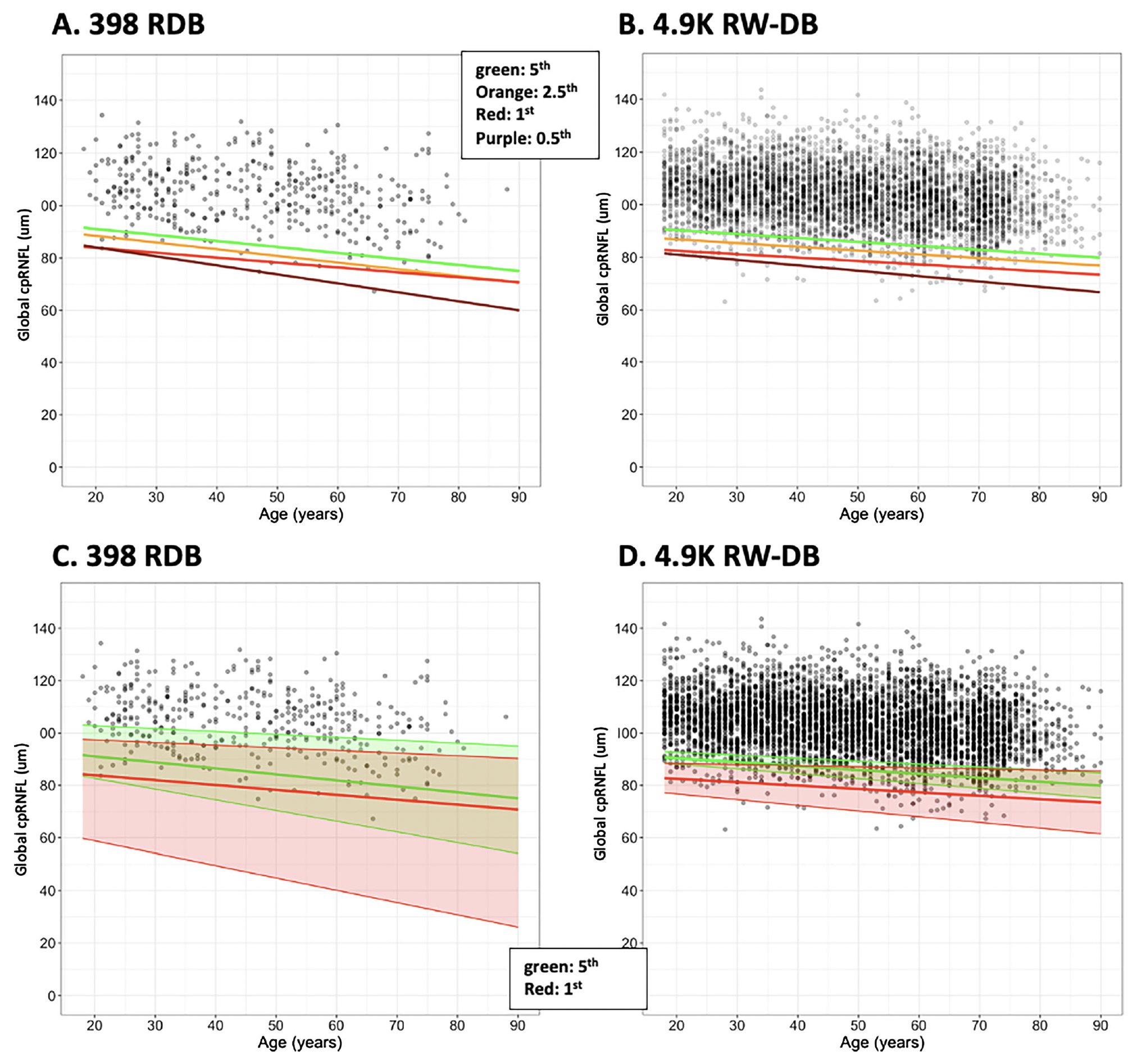
| Using data generated from an independently collected large sample of healthy and diseased eyes from optometric practices could potentially help increase diagnostic accuracy. These plots from the study show how adding to the size of the database tightens the 95% confidence bands: (A) shows cpRNFL thickness of the 398 RDB eyes as a function of age, (B) shows the same as in (A) for the 4,932 RW-RDB eyes, while (C) and (D) show the same data with the regression lines for the 5th (green) and 1st (red) percentile cutoffs and the 95% confidence bands (shaded regions) for these two regression lines. Photo: Hood DC, et al. Transl Vis Sci Technol. 2024;13(10):8. Click image to enlarge. |
The reference databases (RDBs) used in commercial OCT instruments are relatively small, typically around 400 eyes. The small number of eyes in these RDBs limits the analysis of covariates such as age, sex and ethnic background, as well as anatomical parameters such as fovea-to-disc distance and disc area. While a larger sample could mitigate such limitations, the time and cost required to develop a very large reference database are considered unreasonable by many.
A recent study, published in Transitional Vision Science & Technology, detailed how a research team obtained a real-world reference database of healthy OCT reports from approximately 5,000 individuals 18 years and older who were sampled from the database tested at the 10 optometry practices. The team compared this database to a commercial reference database and found that the values of the global circumpapillary retinal nerve fiber layer (cpRNFL) and ganglion cell layer (GCL) thickness metrics, as well as five anatomical parameters, were remarkably similar for both groups. Any statistically significant differences, when present, were minimal and of no clinical significance.
“Given the considerably larger size of the real-world database, these findings have implications for improving accuracy when interpreting results in both clinical settings and clinical trials,” the study authors wrote in their paper.
The real-world RDB of OCT scans from 4,932 eyes from 4,932 individuals was obtained from optometry practices involved in refractive and screening services. These eyes were selected from a larger sample using a reading center approach, which evaluated scan quality and the potential presence of pathology.
This real-world RDB was compared to the Maestro2 (Topcon) commercial reference database of 398 eyes. In particular, the researchers compared the OCT global cpRNFL and global GCL metrics of the real-world reference database as a function of age, along with the distribution of these two metrics and five key anatomical measures known to affect these measures: disc area (mm2), fovea-to-disc distance (mm), location of the superior peak (degrees), location of the inferior peak (degrees) and a proxy for axial length (based on mirror position).
By design, the number of real-world reference database eyes 70 years and older (14.7%) was greater than for the commercial database (10.1%). The error bands on the 5% and 1% quantile regression lines (QRLs) were substantially narrower for the real-world database.
“More accurate cut-off values of healthy eyes, with tighter confidence bands, are thus possible with the larger databases, such as the one proposed here, especially when covariates, such as age and disc size, are needed,” the researchers noted in their paper for TVST. “Given the challenges of scanning older subjects with factors such as smaller pupils, cataracts and epiretinal membranes, we speculate that establishing a separate reference database specifically for those over 70 years of age could significantly increase diagnostic accuracy in this age group.”
Michael Chaglasian, OD, associate professor at Illinois College of Optometry and chief of staff of the Illinois Eye Institute, was the lead author of a 2018 research article detailing the development of a reference database with the Topcon Maestro 3D OCT device. Upon reviewing the findings of the current study, he suggests, “If a real-world model reference database were ever to be adopted by the FDA for OCT devices, it would bring optometric practices—which are the best places to capture this data—into the fold of helping direct how these devices can more accurately separate normal vs. disease in our patients. Optometry is typically not at the table for these types of things.”
The profession, the industry and the general public “will have to sort out how to safely, fairly and appropriately share this wealth of imaging data that is scattered across tens of thousands of practices,” Dr. Chaglasian adds.
Dr. Chaglasian also notes the encouraging findings of this study show that a real-world RDB might offer these benefits compared to traditional databases:
- Larger Sample Size: This study used 10x more subjects than is typical for an OCT database, which enhances the statistical power and reliability of the findings, allowing for more precise estimates of normal parameters and better identification of outliers in the lower end of the normal distribution.
- Diversity of Data: Using optometry practices can lead to a more diverse population sample, helping to ensure that the database reflects a broader range of anatomical and demographic characteristics and making the findings more applicable to real-world clinical settings.
- Improved Accuracy: The larger and more diverse nature of such an approach allows for better characterization of healthy parameters and can improve the accuracy of diagnostic models; for instance, it can help refine the identification of healthy eyes at the lower end of the normal distribution, which is crucial for effective screening and diagnosis.
- Enhanced AI Model Training: The extensive data available can be used to train artificial intelligence models for screening and diagnostic purposes. These models benefit from exposure to a wide range of parameters, which can improve their performance in distinguishing between healthy and diseased eyes.
- Clinical Relevance: The data collected in real-world RDBs is often derived from routine clinical practice, making it more relevant to everyday clinical scenarios.
- Ability to Test Hypotheses: With a larger database, researchers can test more complex hypotheses regarding the relationships between various anatomical parameters and disease states, which may not be feasible with smaller, traditional databases.
| Click here for journal source. |
Hood DC, Durbin M, La Bruna S, et al. Characteristics of a large database of healthy eyes from optometry practices: implications for a real-world reference database. Transl Vis Sci Technol. 2024;13(10):8. |

