 |
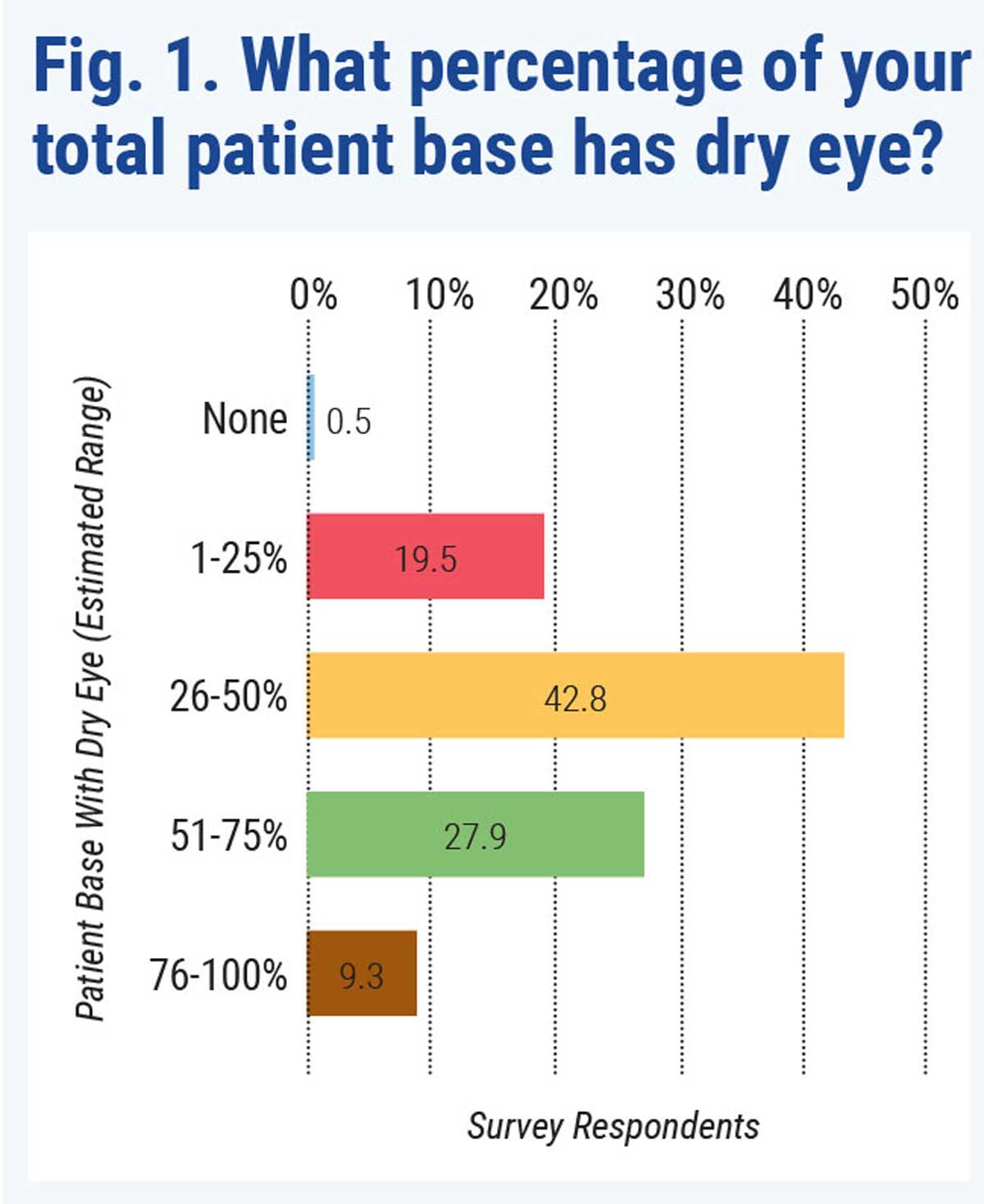
Note: Graph was not from this study. Click image to enlarge. |
New research in mice suggests obstructive sleep apnea (OSA) may be a causative factor of dry eye disease, in which OSA creates abnormal lipid metabolism in the lacrimal glands. In the mouse model, male mice (ages seven to eight weeks) were housed in cages that mimicked OSA using cyclic intermittent hypoxia. The control mice lived in a normal environment.
The researchers reported that the mice in the hypoxic environment had decreased tear secretion, corneal epithelial defects and corneal hypersensitivity. They observed myoepithelial cell damage, abnormal lipid accumulation, reduced cell proliferation, increased apoptosis and inflammatory cell infiltration in the lacrimal gland. They also reported the Hifα and NF-κB signaling pathways were activated and the Pparα was downregulated in the lacrimal glands.
“OSA-induced hypoxia of the lacrimal gland can stimulate Hif1α and Hif2α, further
activate the NF-κB signaling pathway, induce inflammation and downregulate the Pparα signaling pathway,” the researchers proposed in their paper. “This results in abnormal lipid metabolism and mitochondrial dysfunction in lacrimal glands and induces lacrimal gland dyshomeostasis and ROS production, ultimately leading to a reduced aqueous tear secretion and the emergence of attendant dry eye pathological changes.”
They added that fenofibrate treatment significantly alleviated OSA-induced lacrimal gland pathological changes in the mice.
Wang S, He Z, Li Q, et al. Obstructive sleep apnea affects lacrimal gland function. Invest Ophthalmol Vis Sci. 2022;63(3):3. |

