The reason why central corneal thickness (CCT) is connected to glaucoma risk remains unclear. There are no intuitive explanations, because the cornea is not anatomically or physiologically connected to the optic nerve head (ONH), the site of glaucoma damage. Researchers based out of Ohio State University in Columbus recently explored correlations of biomechanical responses between the cornea and the ONH and the peripapillary sclera (PPS) to elevated intraocular pressure (IOP), the primary risk factor for glaucoma.
Using a high-frequency ultrasound elastography technique to image the mechanical responses of the cornea and the ONH/PPS in paired human donor eyes, their study found a strong association between the cornea's shear response and that of the ONH and the peripapillary sclera. Future studies are needed to verify this result in vivo when tools for in vivo characterization of ocular biomechanics become available.
 |
|
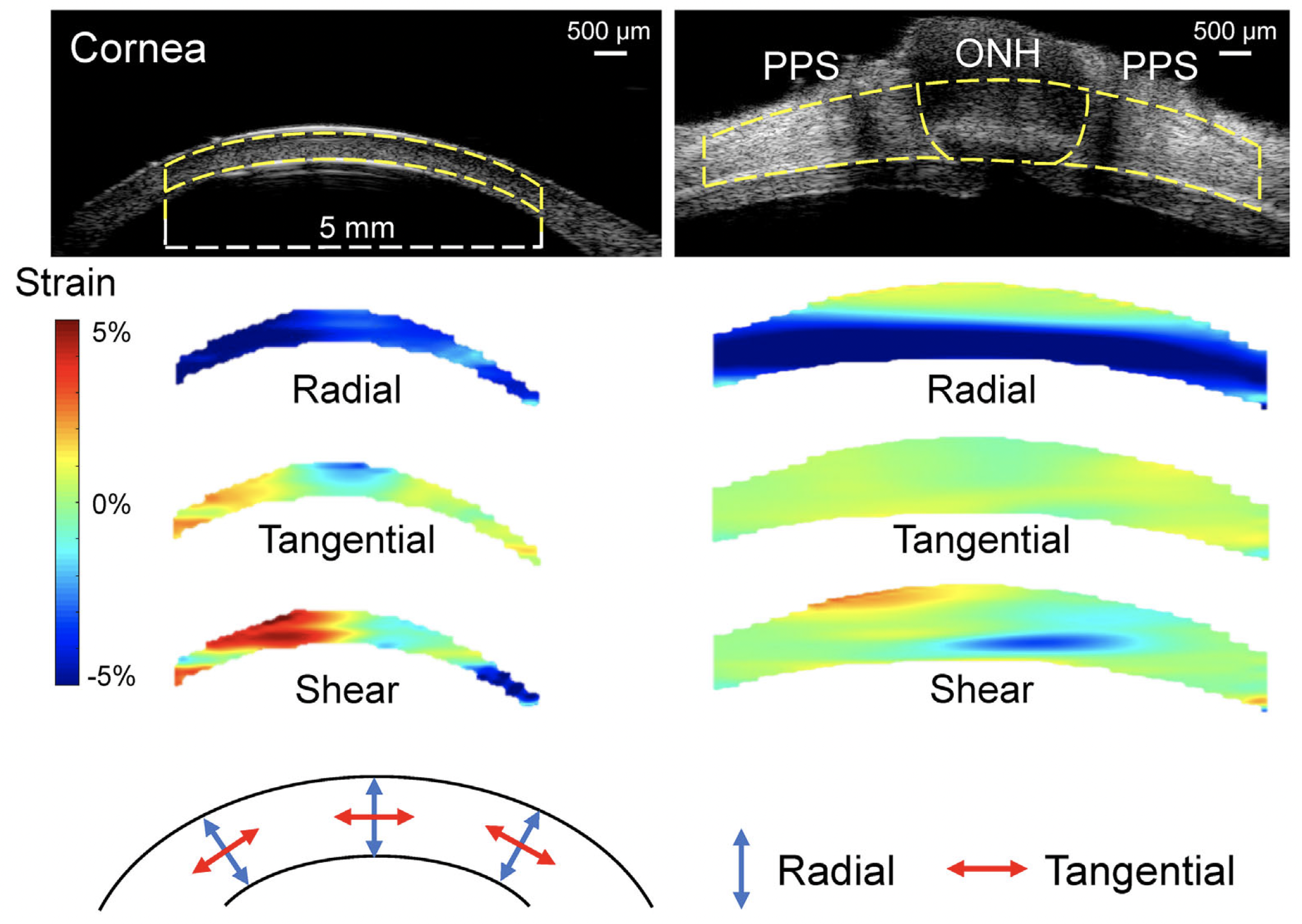
The strong correlation between the cornea’s and the ONH's shear responses to IOP provides new insights and suggests a plausible explanation of the cornea's connection to glaucoma risk. This image from the study shows representative maps of radial, tangential and shear strains in a cornea and a posterior eye of the same donor at 30mm Hg. As the color bar indicates, cyan to blue is negative strain (e.g., compression for radial strain) whereas yellow to red is positive strain (e.g., tensile tangential strain). Dashed yellow lines in the ultrasound images delineate the region of interest for strain analysis. Photo: Pan M, et al. Invest Ophthalmol Vis Sci. 2024;65(5):34. Click image to enlarge. |
Inflation tests were performed on nine pairs of human donor globes. One eye of each pair was randomly assigned for cornea or posterior eye inflation. IOP was raised from 5mm Hg to 30mm Hg at 0.5mm Hg steps in the whole globe, and the cornea or the ONH/peripapillary sclera was imaged using a 50 MHz ultrasound probe. Ultrasound techniques were used to calculate tissue displacements and strains. Associations of radial, tangential and shear strains at 30mm Hg between the cornea and the ONH or peripapillary sclera were evaluated. Corneal shear strain was significantly correlated with ONH shear strain and peripapillary scleral shear strain. CCT was not correlated with any strains in the cornea, ONH or peripapillary sclera.
“The primary finding of this study was that the shear strain in the cornea was strongly correlated with the shear strain in the ONH and peripapillary sclera of the same donor, suggesting a biomechanical correlation between the anterior and the posterior eye,” the authors wrote in their paper for Investigative Ophthalmology & Visual Science. The study did not observe a correlation between CCT and corneal or ONH shear. One possibility was that residual swelling might still be present in some samples during experimentation, which could confound the CCT data.
One of the tested eyes in particular had a large peripapillary scleral shear strain and also a large peripapillary scleral tangential strain. If data from this eye were removed from analysis, correlations between the peripapillary sclera and cornea’s shear and tangential strains would no longer achieve statistical significance. The researchers highlighted that the correlation between ONH and cornea shear strains remains significant after removing data from this eye. Interestingly, the peripapillary sclera was abnormally thin in this eye (approximately 582µm), suggesting a potential relationship between thin PPS and large PPS shear/tangential strains in response to IOP.
“The correlation between the cornea and the ONH/peripapillary sclera's shear response provides a possible explanation for the connection between the cornea and glaucoma, suggesting that an eye that experiences a larger shear strain in the cornea would also experience a larger shear strain in its ONH/peripapillary sclera at an increase in IOP, which could contribute to glaucoma damage,” they noted. “Understanding such a connection will further elucidate the mechanisms and risk factors underlying glaucoma and provide new insights to improve the diagnosis and treatment of this debilitating disease.”
Pan M, Kwok S, Pan X, Liu J. Biomechanical correlations between the cornea and the optic nerve head. Invest Ophthalmol Vis Sci. 2024;65(5):34. |

