 |
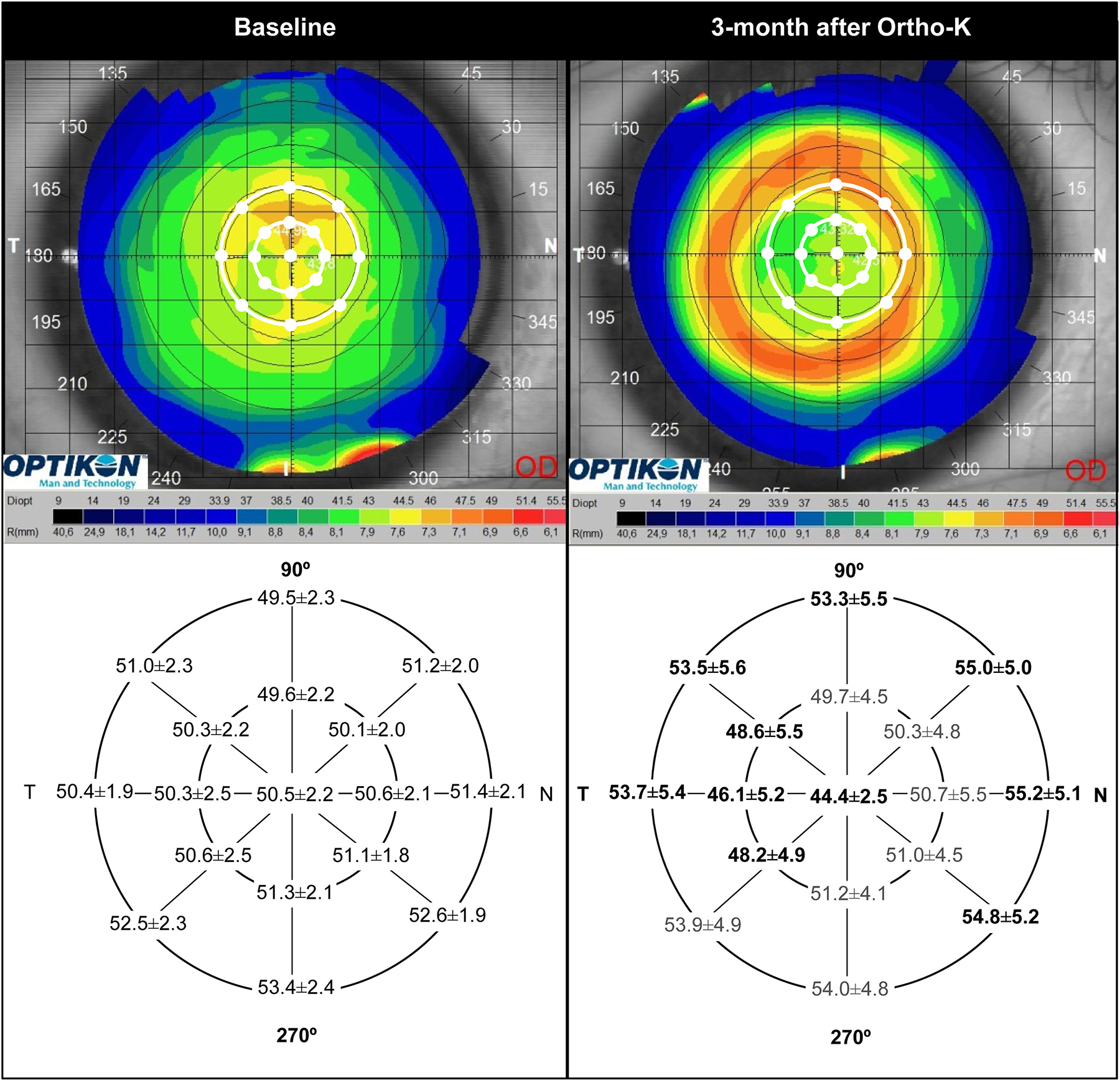
Corneal topography and epithelial thickness changes between baseline (left) and after three-month ortho-K treatment period (right). Note the stronger central and temporal epithelial thinning, and highest mid-peripheral thickening corresponding to nasal area in clear association with temporal decentration observed in this study (Figure from the study, used under Creative Commons 4.0). Photo: González-Pérez J et al. J Optom. 2023;17(2). Click image to enlarge. |
Orthokeratology (ortho-K) has fully established itself as a mainstay treatment for myopia management over the years and especially more recently. Researchers have conducted many studies about the intervention’s effects on the eye itself. In one recent report, investigators wanted to elucidate the topographic epithelial and total corneal thickness changes in myopic patients using ortho-K lenses in connection with objective contact lens decentration assessment.
The prospective study included 32 Caucasian myopic eyes undergoing ortho-K for three months. OCT angiography was used to measure total, epithelial and stromal thicknesses both before and after treatment, as well as central, paracentral and mid-peripheral values taken along eight semi-meridians.
After ortho-K wear, average total central corneal thickness was 4.7µm±1.0µm thinner. Paracentral corneal thickness did not change, but mid-peripheral corneal thickness did increase by 3.3µm ±1.6µm, exclusive linked to the epithelial plot. Lens fitting decentration of less than 1.0mm was found in the entire sample, with most exhibiting horizontal-temporal type (87.5%) and vertical-inferior making up half (50%). Analysis of corneal topography showed a horizontal and vertical epithelial thickness asymmetric change profile with paracentral temporal thinnest values, while mid-peripheral nasal values were thickest.
Elucidating their findings, the study researchers explain that mid-peripheral thickening seems to be mainly epithelial in origin. Elaborating more, the authors relay that the observed central corneal thinning is consistent with previous literature, while mid-peripheral corneal thickness changes present some controversy in relation with stromal contribution. Despite these observed effects, their mechanisms are unclear. One study looked at tear samples of ortho-K wearers for molecular analysis, finding increased metalloproteinase MMP-9 and epidermal growth factor levels, both of which contribute to cellular redistribution and are linked with reparative corneal response. As such, the mid-peripheral thickening coupled with central thinning may be a process of epithelial redistribution from center to limbus.
Stromal thickening has been observed in some studies and not in others. This study found only a trend of stromal thickening (+3.9%) in the paracentral area, reflecting other research that did not find mid-peripheral stromal changes.
This study also observed epithelial thickness changes along both horizontal and vertical meridians. The horizontal differences are similar to another recent study, but the vertical differences with epithelial thickening only in superior zones are newly described.
Finally, the observation that lens decentration tended to move temporally and inferiorly is consistent with previous studies, too. Vertical lens decentration was not associated with regional epithelial or stromal changes; however, post ortho-k epithelial changes were linked with the magnitude of horizonal lens decentration. The horizontal magnitude was also positively associated with mid-peripheral epithelial changes (nasal and superior) and negatively associated with mid-peripheral temporal epithelial changes.
Clinically, the authors “affirm that for better monitoring redistribution of corneal tissue in subjects undergoing ortho-K, it would be desirable to have instruments that allow an automated larger analysis area, covering at least the central 8mm of the cornea, which is not possible with most of the current AS-OCT systems.”
González-Pérez J, Sánchez-García A, Parafita MA. Epithelial and stromal thickness profile and lens decentration in myopic orthokeratology. J Optom. 2023;17(2). [Epub ahead of print]. |

