 |
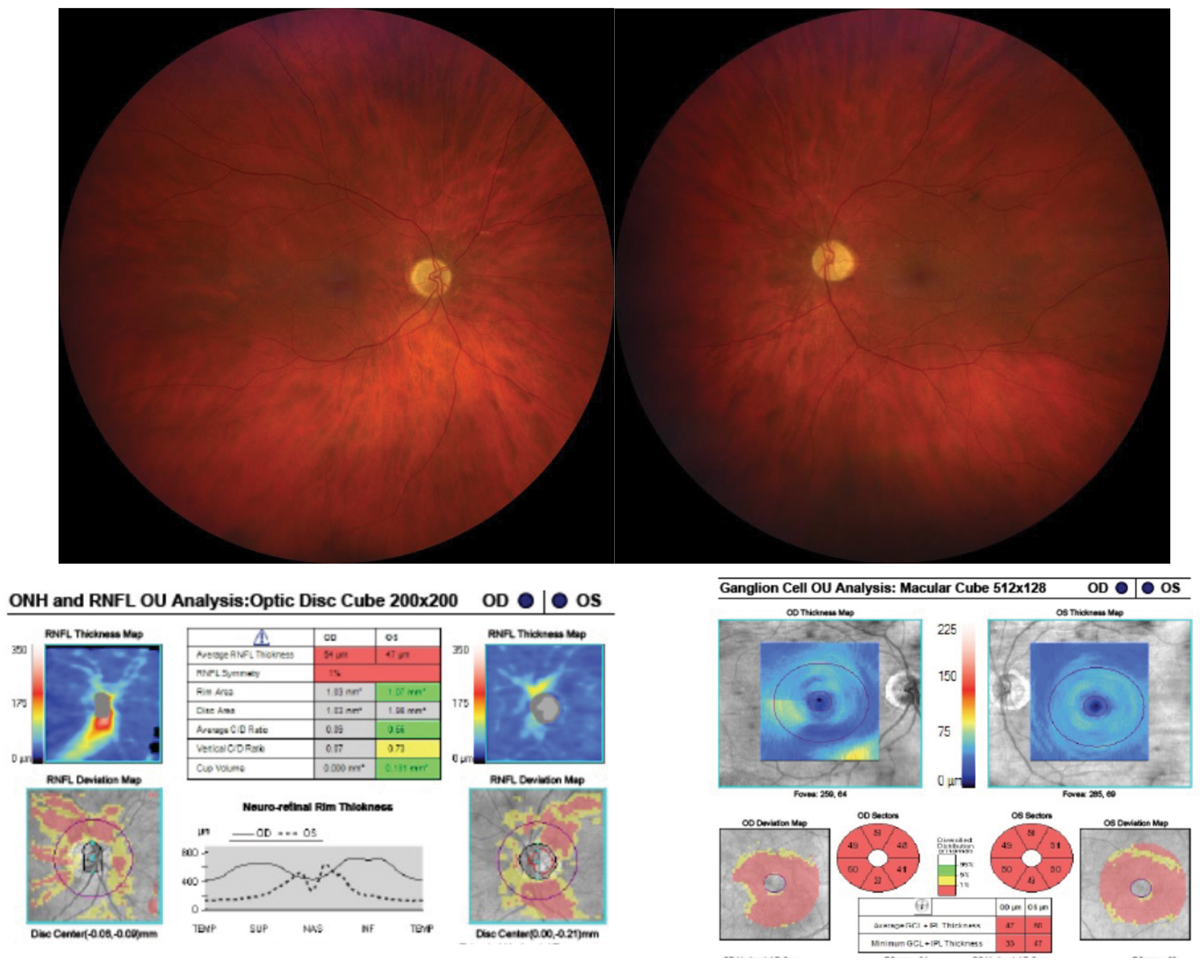
| Although relative afferent pupillary defect (RAPD) presence is more commonly associated with asymmetric optic neuropathy, maculopathies can result in RAPD if associated with extensive asymmetric retinal damage. Photo: Marc D. Myers, OD. Click image to enlarge. |
Clinical features of conditions affecting the macula and optic nerve can overlap, and both can possibly present with decreased visual acuity and variable color vision loss. Because of these overlapping symptoms, maculopathy can go misdiagnosed as optic neuropathy, ultimately leading to patient harm. With this in mind, researchers wanted to investigate which specific findings or tests were best able to parse out one condition from the other.
A retrospective chart review included consecutive patients over 4.5 years who were referred to neuro-ophthalmology clinics with an optic neuropathy diagnosis but were ultimately diagnosed with maculopathy. Included was a total of 47 patients, of which 27 were female and median age was 55 years, ranging from 18 to 85. The majority of referrals to neuro-ophthalmology were from ophthalmologists (72.3%) and then optometrists (12.8%). Results were published last week in Journal of Neuro-ophthalmology.
Maculopathy diagnosis was possible upon the first neuro-ophthalmic consultation in 51.1% of cases. Relative afferent pupillary defect was present in only 6.4% (three) patients, while benign disc anomalies of tilted, myopic, small or anomalous discs were present in 34.0%, with 21.3% displaying pathologic disc changes unrelated or secondary to maculopathy. Tellingly, macular OCT was abnormal in 84.4%, with outer retinal pathology in 42.2% and inner retina pathology in 17.8%. At a similar rate, retinal nerve fiber layer (RNFL) thickness was normal in 82.6% of patients.
Subsequently, the researchers specify that macular cone dystrophies, unspecified retinal disorders and macular degeneration were the most common mimickers of optic neuropathy. They also point to coexistent benign and pathological disc anomalies contributing to the misdiagnosis of maculopathy as optic neuropathy.
Of the 27.7% of patients who received neuroimaging before referral, 23.0% were done with contrast. However, all patients that did have prior neuroimaging done could have received the correct diagnosis at first neuro-ophthalmic consultation through clinical examination and peripapillary and/or macular OCT only.
The study authors relay that “this finding emphasizes the importance of skilled neuro-ophthalmic examination in making the final diagnosis in patients presumed to have optic neuropathy and its ability to obviate the need for neuroimaging in these patients, thus conserving healthcare resources and eliminating patients’ anxiety.” What’s more, non-specialists should be aware that contrast administration during neuroimaging for suspected optic neuropathy can rule out inflammatory or compressive etiologies of the condition, they advised in their article.
The authors also elaborate that presenting symptoms and time course can cue one in on distinguishing maculopathy from optic neuropathy. Ischemic optic neuropathies and optic neuritis typically display acute or subacute presentation, while hereditary and compressive optic neuropathies, like maculopathies, are onset more insidiously.
Optic neuropathies typically have greater decrease in central visual acuity, have associated relative afferent pupillary defect and greater color sensitivity reduction, while maculopathies typically present with color vision reduction associated with the degree of central vision loss, except in cases of cone dystrophies. Keeping with the known characteristics of maculopathy, most patients (70.2%) had chronic symptom onset, preserved visual acuity and only six patients had color vision deficits.
Since a thinning RNFL and ganglion cell inner plexiform layer are more indicative of optic neuropathy than normal RNFL, and this study’s authors found normal RNFL thickness in most patients, they suggest that “macular OCT is a high-yield test in differentiating between optic neuropathy and maculopathy and should be obtained in patients with suspected optic neuropathies who have normal RNFL thickness.”
Vosoughi AR, Donaldson L, Micieli JA, Margolin EA. Maculopathies referred to neuro-ophthalmology clinic as optic neuropathies: a case series. J Neuro-Ophthalmol. 2023. [Epub ahead of print]. |

