Death and taxes aside, there are some fundamental truths of life. For one, the number of presbyopes and myopes is increasing.1 The global prevalence of presbyopia was estimated at 1.8 billion (25%) in 2015 and is anticipated to peak in 2030.1 The population of Americans 65 and older is projected to roughly double between 2010 and 2050.2 Myopes are estimated to represent 49.8% by 2050, posing increasing economic burdens on society.2-6
Lens Evolution
Not only do presbyopes and myopes share common epidemiological trends, but overlaps also exist in the evolution of corrective options. Surgical and non-surgical innovations have progressed in tandem, albeit at different rates. LASIK refractive surgery arose first to treat myopia. Some are using it successfully to create a monovision effect. More recently, its expanded indications include presbyopia, leading to the development of such terms as presby-LASIK.7-11 Intraocular lenses (IOLs) initially corrected only the spherical component of patients’ refractive errors. These now include toric, multifocal (bifocal, trifocal and aspheric), toric-multifocal and accommodating options.12-18 Diffractive lens options continued to evolve and the next development is extended depth-of-focus (EDOF) designs.13 But it has branched off in a few other areas, too.
Corneal inlays, for example, are another alternative surgical approach to managing presbyopia. Currently available inlays include the Flexivue Microlens (PresbiBio) and the Kamra inlay (CorneaGen).19-21 A third option—the Raindrop Near Vision Inlay (ReVision Optics)—was recently recalled by the FDA following the shuttering of its parent company.
Alternative explanations to Helmholtz’s theory on how accommodation occurs have led to scleral banding or expansion procedures to modestly restore some level of accommodation as well.22 These alternative theories are not generally accepted.
Noninvasive procedures include a host of contact lens designs. Rigid, soft and hybrid lenses now offer multifocal designs. Rigid lenses are available in simultaneous and alternating designs while soft and hybrid lenses come in simultaneous view designs. Alternating designs in soft lenses such as the Triton lens (Gelflex) and the first diffractive bifocal, Echelon (Hydron), are no longer available, but are interesting historical footnotes.23 Contemporary soft simultaneous vision contact lenses exist as aspheric, zonular and EDOF designs. This last design is what we will concentrate on and is of particular interest for its novel attributes.
Various topical pharmaceutical agents are also in development with varying mechanisms of action and are worth a passing mention; these expand depth-of-focus by creating a pinhole effect or restore some measure of flexibility to the aging crystalline lens.24
Considerable time and treasure are required to address the impact of both presbyopia and myopia by improving access to care and developing timely interventions to slow myopia’s progression. This article seeks to update practitioners on EDOF by drawing parallels across corrective options.
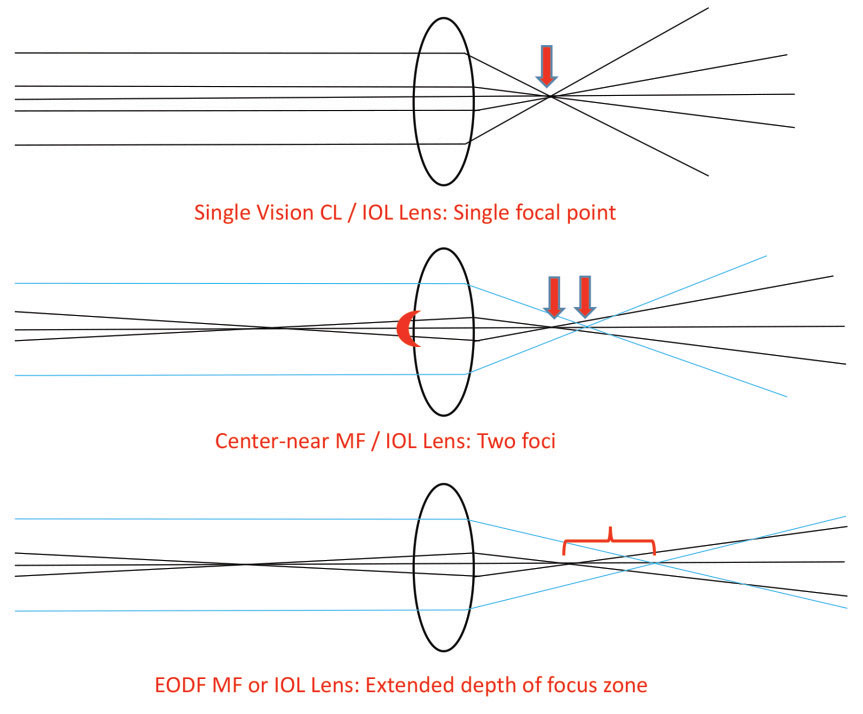 |
| Fig. 1. A single vision lens produces a single focal point (top). A near-centered multifocal lens (MF) simultaneously creates superimposed images of distance and near zone foci (middle). Extended depth-of-focus (EDOF) lenses broaden the depth of focus to encompass a broader range of foci (bottom). The model assumes a monochromatic light source and paraxial rays to avoid confounding aberrations and for simplicity. |
Optical Basics
Obtaining a single point focus can be challenging when light from an object passes through corrective lenses and the optics of the eye. When a wavefront of light encounters an optical surface, three things happen: reflection, absorption and transmittance. Also, individual wavelets join to create a wavefront that is diffracted when it encounters the edge of an aperture such as the iris plane, resulting in interference. The transmitted wavefront from a point object would ideally be conjugate with that of a point image. We live in a world of polychromatic light with both paraxial and off-axis objects. The wavefronts created encounter both regular and irregular optical surfaces, resulting in a difference between the ideal and actual wavefronts we refer to as aberrations. These are the optical aberrations of refracting surfaces, which smear the focus light.
Aberrations may be characterized into lower- and higher-order ones. Lower-order aberrations represent approximately 90% of those in the eye and include the defocus errors (myopia, hyperopia, regular astigmatism and prism) we correct every day by refraction.25 Higher-order aberrations account for the other 10% of the eye’s errors and often influence the quality of patient’s vision after optical or surgical intervention.26 The clinically most important ones are spherical aberration, coma and trefoil.27
Because spherical aberration increases as the fourth power of the pupil diameter, the aberration will increase 16 times the change in diameter.25 This is one reason why patients with large pupils who receive LASIK may complain of halos and it is responsible for night myopia in normal eyes.26 Accommodation and IOL axial placement relative to the pupillary aperture affect spherical aberration as well.25 If a corneal graft, crystalline or intraocular lens, inlay or ablation zone is decentered, coma increases. Trefoil contributes a minor part to image aberration.28
Correcting refractive defocus is a major factor in reducing the smear of a point focus. The shapes of refracting surfaces, aperture size and position of the elements in an optical system both axially and longitudinally affect higher aberrations and quality of vision significantly.
Management of allergic eye diseases, including seasonal, atopic and vernal keratoconjunctivitis, should focus on treating both chronic symptoms and acute flares. Patients should avoid allergens and employ supportive care such as cool compresses and ocular lubrication to improve symptoms. Artificial tears not only lubricate the ocular surface, but can dilute pathogens and decrease itching. Topical H-1 receptor antagonists, mast-cell stabilizers or combination drops can control itching in seasonal and vernal keratoconjunctivits, but are less effective in AKC. For severe AKC, topical treatment with cyclosporine drops or tacrolimus is warranted. Topical corticosteroids may be indicated for exacerbations but are not recommended for long-term use due to side effects. Vasoconstrictor drops should be avoided in allergic eye disease due to rebound hyperemia.
Intraocular Lenses
Until we perfect devices to simulate accommodation or restore natural accommodation, we must accept the inherent trade-offs present in all technologies. The key is to match the right option to an individual patient by considering lifestyle needs, comorbidities and an evidence-based approach (Figure 1).12
The majority of multifocal IOLs are refractive, diffractive and EDOF. The only FDA-approved EDOF lens available in the United States is the Tecnis Symfony (Johnson & Johnson).29 A pinhole aperture design, the ICD-8 (AcuFocus), also provides EDOF; it recently received investigational device exemption and is currently enrolling study patients.30
The European Union has three offerings in this space:31
- The Mini Well (Sifi Medtech)
- The Wichterle Intraocular Lens-Continuous Focus (Medicem)
- The XtraFocus Pinhole Implant (Morcher)
These various designs have their own advantages. Important clinical outcomes include uncorrected distance, intermediate and near visual acuities, spectacle independence and patient satisfaction. A 2017 literature search included 74 studies that provide insights into the efficacy of multifocal IOLs.12 The results show the overall superiority of monocular visual acuity at all distances in diffractive designs over multifocal designs, though both performed worse in the intermediate and near ranges than at distance.12,32 However, when spectacle independence (defined as free of use at least 80% of the time) was assessed globally at distance (96.0%), intermediate (100%) and near (70%), results suggested patients are largely able to make successful neuro-adaptations.12
The most commonly reported symptoms among dissatisfied patients wearing multifocals (1.3%), diffractive (2.6%) or combined designs (91.1%) are blurred vision (94.7% to 95%) and photic complaints (38.2% to 42%).33,34 The causes of dissatisfaction reported included residual ametropia (65.5%), posterior capsular opacification (15.8%), large pupil size (14.5%) and wavefront abnormalities (11.8%).34 To put some of this in perspective, a Cochrane meta-analysis suggested photic complaints are two to two and a half times more common in multifocal than in single vision IOLs.35 Many causes of the reported blur are easily ameliorated.12,32-34,36
EDOF and trifocal designs outperform bifocal designs in optical bench testing of through focus clarity.37 This demonstrates how the distance focus extends into the intermediate range for both EDOF and trifocals with better intermediate focus for EDOF designs and slightly better near range for the trifocal design tested.14,37-40 There is no significant difference for halos or glare complaints (10% to 64%) between the two.37,41,42
Comparisons of EDOF with bifocal and trifocal designs for visual acuity are lacking. Small sample outcomes evaluating bilateral implants for subjects attaining uncorrected logMAR visual acuities of better than 0.1D (20/25) have been reported as distance (100%), intermediate (92% to 100%) and near (40%).43 The results are inherently better than those reported above since they represent binocular findings. Nonetheless, these studies provide some insights into the efficacy of various designs. One recent study compared outcomes between four different lenses: Tecnis 1-piece monofocal, Tecnis Symfony extended range of vision, Restor +2.5D and Restor +3.0D. That study found Tecnis Symfony extended range of vision IOL and +2.5D multifocal IOL provided significantly better intermediate visual restoration after cataract surgery than the monofocal IOL or +3.0D multifocal IOL, with significantly better quality of vision with the Tecnis Symfony.
The largest study to date evaluating the ICD-8 design enrolled 105 subjects who received this lens in one eye and a monofocal design in the opposing eye. They were evaluated over a six-month period, finding uncorrected binocular Snellen visual acuities at distance (20/23), intermediate (20/24) and near (20/30) with 95.9% indicating they would have the procedure again.45
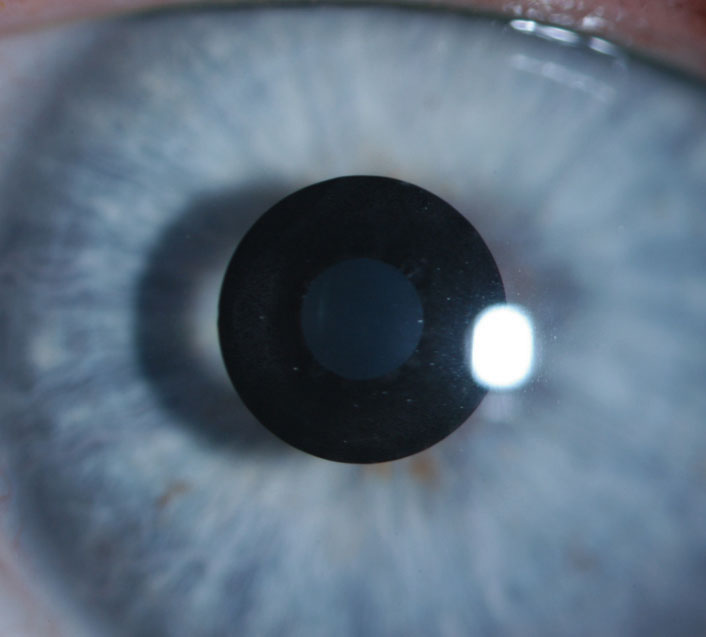
 |
| Retro-illumination of the Tecnis Symfony. Photo by Yueren Wang, OD. |
Corneal Inlays
The intracorneal inlays for presbyopia on the market are the Kamra and Flexivue Microlens.46 However, only the Kamra inlay uses an EDOF mechanism of action.28
The Kamra inlay is one of the most studied inlays in this category, with more than 20,000 implanted in more than 50 countries.30,47 The use of a pinhole approach to extend the depth of focus preserves distance vision and binocularity over a broad range of focus.20 The lens is inlayed in the non-dominant eye only, preferably into a femtosecond laser pocket to maximally preserve corneal nerve integrity.20 This reduces the risk of creating dry eye issues.48 It has been used in myopes, emmetropes, hyperopes, LASIK, monofocal pseudophakes and phakic IOL patients and shows its best results in myopes less than -1.00D and less than -0.75D of astigmatism.20
The outcomes are positive overall. In general, practitioners may expect a slight decrease in uncorrected distance visual acuity, stable or improved uncorrected intermediate visual acuity, and great improvement in uncorrected near visual acuities. The greatest gains at near are for hyperopes, emmetropes and myopes, in that order. Best-corrected visual acuities are rarely affected unless explantation becomes necessary or complications arise.49-54 Contrast sensitivity does not appear to be affected in most of these studies, but higher-order aberrations can increase if the corneal thickening alters the corneal topography. This is uncommon at the depth the inlay is placed.
Complications are rare. They include those associated with refractive surgery and femtosecond laser procedures. Those unique to this procedure include epithelial flattening secondary to stromal thickening with concomitant hyperopic shift; corneal haze, epithelial iron deposits and microbial keratitis.50 Other reported complications were more common with the original design, (ACI 7000), and were minimized with the reduction in light coming through the aperture in the newer smaller-aperture design as well as by increasing in the number of fenestrations to the aperture in the thinner design (ACI 7000 PDT).49,50 The complications include severe night vision complaints, dependence on spectacles at near, loss of best-corrected distance visual acuity of one line, rare decentration and epithelial deposits with the first generation version.49,50
Contact Lens Options
The only commercially available EDOF contact lens in the United States is the NaturalVue Multifocal 1 Day (Visioneering Technology) soft lens, which uses what the company calls neurofocus optics.55 This novel design offers an “encompassing” add range up to +3.00D by taking advantage of EDOF optics.55 This is important not only for presbyopes but for myopes.56,57 It is effectively a center-distance design with increasing add power moving outward from the center.
Prototypes of a similar design have been studied by researchers at the Brien Holden Vision Institute (BHVI).58-63 The base curve is a little flatter (8.4mm) and the diameter a little smaller (14.0mm) than the NaturalVue Multifocal.
The goal of these designs is to circumvent the common complaints and issues previously cited as shortfalls of simultaneous view designs such as ghosting, decreased quality of vision, decreased contrast sensitivity, the undue influences of pupil size, centration and illumination levels.58
The BHVI design has a low and high add, and was compared with a center-distance, zonular design.58 Its EDOF design performed better in the intermediate and near zones without visual compromise in the distance compared with the zonular design.58
Another study compared predicted outcomes for a through focus design with low, medium and high add powers using a computer model for presbyopic emmetropes, against center-distance, zonular and center-near simultaneous view designs.59 They found EDOF designs to be less susceptible to variations in pupil size, inherent ocular aberration and decentration relative to concentric or simultaneous view designs, and included the caveat that human trials are needed to further test their results.59 This was tested in a prospective, participant-masked, crossover randomized study on a range of refractive errors and add powers.60 Each lens was worn for approximately one week. They found results similar to those predicted by the through focus models and consistent with two other short-term comparisons to the same center-distance, zonular and near-center, aspheric simultaneous view designs worn on a daily basis.60-62 The prototype in this study had a slightly flatter base curve (8.5mm) and larger diameter (14.2mm) than either the through focus part 1 or part 2 studies.59,60,62
Taken together, these results suggest EDOF designs may offer advantages over both center-distance, zonular and more common, center-near, simultaneous view designs for presbyopia.
 |
| A patient presents with an otherwise quiet and clear cornea at 12 months after Kamra inlay implantation. Photo by Clark Chang, OD. |
Myopic Defocus
This section concentrates on the ability of EDOF lenses to create peripheral myopic defocus.64 Mounting evidence suggests induced myopic retinal defocus (especially peripheral) may slow myopia progression significantly by ill-defined control mechanisms, which influence scleral thickness and rigidity.64-77 Soft contact lens designs studied include bifocals, peripheral defocus, simultaneous dual focus, positive spherical aberration and EDOF ones. They are capable of reducing both spherical equivalent error and, more importantly, axial length, with fewer adverse events or complications than atropine or orthokeratology.56,78 Little is known about rebound after discontinuation of wear or which groups (slow or fast progressors) benefit most.56 Early intervention appears particularly beneficial in fast progression.79 Epidemiological data suggests a reduction in progression of myopia by 50% or more significantly reduces the burden of high myopia and its complications.3,80,81
A prospective, double-blind, crossover, randomized one-week trial of the EDOF BHVI prototype was compared against the dual focus design MiSight (CooperVision) and Proclear Multifocal (CooperVision) for tolerability in 30 subjects.63 The findings suggested EDOF designs are better tolerated than the two designs often advocated for myopia control. Tolerability is important, but what about efficacy? The authors of the study cite a combination of peer-reviewed data and poster abstracts to compare some short-term data for efficacy.
The NaturalVue Multifocal center-distance lens design offers “approximately 8D to 11D of relative plus power at the edge of the pupil and approximately 20D of relative plus power at the edge of the optic zone.”57 A 2018 study reported on a multi-site, retrospective case series collating data from 32 consecutive patients with at least one six-month follow-up visit.57 The majority, 93.6%, wore the lenses for 18 months or less. They reported seemingly impressive reductions in myopic progression of 95% or more and even suggested regression occurred in some subjects when compared with progression rates prior to using the EDOF design.57
All studies have limitations created by design differences, which prevent direct comparisons. Studies using case series represent relatively low-level evidence. The lack of masking, use of historical controls, lack of randomization, lack of axial length data, varying lengths of subject participation and small sample sizes are limiting.57 Nonetheless, the results are promising.
Clearly, interest in EDOF optics continues to grow, and its applications across a variety of platforms offer some advantages over other designs. It is worth your time to keep abreast of these developments and add them to your clinical toolbox for presbyopes and as off-label treatment for myopia progression.
Dr. Fuller is an associate professor and founding supervisor of the Cornea & Contact Lens – Refractive Surgery residency at The Eye Center, Southern College of Optometry.
| 1. Fricke T, Tahhan N, Resnikoff S, et al. Global prevalence of presbyopia and vision impairment from uncorrected presbyopia: Systematic review, meta-analysis, and modelling. Ophthalmol. 2018;125(10):1492-9. 2. Vincent G, Velkoff V. The next four decades the older population in the United States: 2010 to 2050. Curr Pop Report. www.census.gov/prod/2010pubs/p25-1138.pdf. May 2010. Accessed March 11, 2019. 3. Holden B, Fricke T, Wilson D, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmol. 2016;123(5):1036-42. 4. Frick K, Joy S, Wilson D, et al. The global burden of potential productivity loss from uncorrected presbyopia. Ophthalmol. 2015;122(8):1706-10. 5. Holden B, Fricke T, Ho S, et al. Global vsion impairment due to uncorrected presbyopia. Arch Ophthalmol. 2008;126(12):1731. 6. Sade RM. The graying of America: challenges and controversies. J Law Med Ethics. 2012;40(1):6-9. 7. Vargas-Fragoso V, Alió J. Corneal compensation of presbyopia: PresbyLASIK: an updated review. Eye Vis. 2017;4:11. 8. Pallikaris I, Panagopoulou S. PresbyLASIK approach for the correction of presbyopia. Curr Opin Ophthalmol. 2015;26(4):265-72. 9. Mosquera SA, Alió JL. Presbyopic correction on the cornea. Eye Vis. 2014;1:5. 10. Luger M, McAlinden C, Buckhurst P, et al. Presbyopic LASIK using hybrid bi-aspheric micro-monovision ablation profile for presbyopic corneal treatments. Am J Ophthalmol. 2015;160(3):493-505. 11. Schlote T, Heuberger A. Multifocal corneal ablation (Supracor) in hyperopic presbyopia: 1-year results in a cross-sectional study. Eur J Ophthalmol. 2017;27(4):438-42. 12. Alio J, Plaza-Puche A, Férnandez-Buenaga R, et al. Multifocal intraocular lenses: An overview. Surv Ophthalmol. 2017;62(5):611–34. 13. Chang D, Huggins L. Understanding the role of IOL optics in postoperative vision complaints. Rev Optom. 2018;155(12):48–51. 14. Zvornicanin J, Zvornicanin E. Premium intraocular lenses: The past, present and future. J Curr Ophthalmol. 2018;30(4):267-96. 15. Gundersen K. Rotational stability and visual performance 3 months after bilateral implantation of a new toric extended range of vision intraocular lens. Clin Ophthalmol. 2018;12(7):1269-78. 16. Alió J, Simonov A, Romero D, et al. Analysis of accommodative performance of a new accommodative intraocular lens. J Refract Surg. 2018;34(2):78–83. 17. Ong H, Evans J, Allan B. Accommodative intraocular lens versus standard monofocal intraocular lens implantation in cataract surgery. Cochrane Database Syst Rev. 2014 May 5;CD009667. 18. Zhou H, Zhu C, Xu W, Zhou F. The efficacy of accommodative versus monofocal intraocular lenses for cataract patients. 2018;97(40): p e12693. 19. Binder PS. Intracorneal inlays for the correction of presbyopia. Eye Contact Lens. 2017;43:267-75. 20. Moarefi MA, Bafna S, Wiley W. A review of presbyopia treatment with corneal inlays. Ophthalmol Ther. 2017;6(1):55-65. 21. Konstantopoulos A, Mehta JS. Surgical compensation of presbyopia with corneal inlays. Expert Rev Med Devices. 2015;12(3):341–52. 22. Kleinmann G, Kim HJ, Yee RW. Scleral expansion procedure for the correction of presbyopia. Int Ophthalmol Clin 2006;46(3):1–12. 23. Rex Ghormley N. The hydron ECHELON bifocal contact lens. Int Contact Lens Clin. 1989;16(4):315-7. 24. Cole J. Can an eyedrop eliminate presbyopia? Rev Optom. 2017;154(6):42-6. 25. Lombardo M, Lomabard G. Wave aberration of human eyes and new descriptors of image optical quality and visual performance. J Cat Refract Surg. 2010;36(2):313-31. 26. Bruce A, Catania L. Clinical applications of wavefront refraction. Optom Vis Sci 2014;91(10):1278-86. 27. Lawless M, Hodge C. Wavefront’s role in corneal refractive surgery. Clin Exp Ophthalmol. 2005;33(2):199-209. 28. Appelgate R, Sarver E, Khemsara V. Are all aberrations equal? J Refract Surg 2002;18(5):S556-62. 29. Johnson & Johnson Vision. TECNIS Symfony IOL | Johnson & Johnson Vision. Packag Inser 2018. 30. AcuFocus. Improving Lifestyle Vision with Small Aperture Optics. Irvine; 2016. 31. Akella SS, Juthani V. Extended depth of focus intraocular lenses for presbyopia. Curr Opin Ophthalmol. 2018;29(4):318–22. 32. Rosen E, Alió J, Dick H, et al. Efficacy and safety of multifocal intraocular lenses following cataract and refractive lens exchange: Metaanalysis of peer-reviewed publications. J Cataract Refract Surg. 2016;42(2):310-28. 33. de Vries NE, Webers CAB, Touwslager W, et al. Dissatisfaction after implantation of multifocal intraocular lenses. J Cataract Refract Surg. 2011;37(5):859–65. 34. Woodward M, Randleman J, Stulting R. Dissatisfaction after multifocal intraocular lens implantation. J Cataract Refract Surg. 2009;35(6):992–7. 35. Calladine D, Evans J, Shah S, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2012 Sept;9:CD003169. 36. de Vries N, Nuijts R. Multifocal intraocular lenses in cataract surgery: Literature review of benefits and side effects. J Cataract Refract Surg. 2013;39(2):268-78. 37. Gatinel D, Loicq J. Clinically relevant optical properties of bifocal, trifocal, and extended depth of focus intraocular lenses. J Refract Surg. 2016;32(4):273-80. 38. Ruiz-Mesa R, Abengózar-Vela A, Aramburu A, Ruiz-Santos M. Comparison of visual outcomes after bilateral implantation of extended range of vision and trifocal intraocular lenses. Eur J Ophthalmol. 2017;27(4):460–5. 39. Yoo Y, Whang W, Byun Y, et al. Through-focus optical bench performance of extended depth-of-focus and bifocal intraocular lenses compared to a monofocal lens. J Refract Surg. 2018;34(4):236-43. 40. Cochener B, Boutillier G, Lamard M, Auberger-Zagnoli C. A comparative evaluation of a new generation of diffractive trifocal and extended depth of focus intraocular lenses. J Refract Surg. 2018;34(8):507-14. 41. de Medeiros AL, de Araújo Rolim AG, Motta AFP, et al. Comparison of visual outcomes after bilateral implantation of a diffractive trifocal intraocular lens and blended implantation of an extended depth of focus intraocular lens with a diffractive bifocal intraocular lens. Clin Ophthalmol. 2017;11(10):1911–6. 42. Savini G, Balducci N, Carbonara C, et al. Functional assessment of a new extended depth-of-focus intraocular lens. Eye (Lond). 2019;33(3):404-10. 43. Ganesh S, Brar S, Pawar A, Relekar KJ. Visual and refractive outcomes following bilateral implantation of extended range of vision intraocular lens with micromonovision. J Ophthalmol. 2018;2018. 44. Pedrotti E, Carones F, Aiello F, et al. Comparative analysis of visual outcomes with 4 intraocular lenses: Monofocal, multifocal, and extended range of vision. J Cataract Refract Surg. 2018;44(2):156–67. 45. Dick H, Piovella M, Vukich J, et al. Prospective multicenter trial of a small-aperture intraocular lens in cataract surgery. J Cataract Refract Surg. 2017;43(7):956–68. 46. Mehrjerdi M, Mohebbi M, Zandian M. Review of static approaches to surgical correction of presbyopia. J Ophthalmic Vis Res. 2017;12(4):413-8. 47. Lindstrom R, Macrae S, Pepose J, Hoopes P. Corneal inlays for presbyopia correction. Curr Opin Ophthalmol. 2013;24(4):281–7. 48. Efron N, Jones L, Bron A. The TFOS International workshop on contact lens discomfort: report of the contact lens interactions with the ocular surface and adnexa subcommittee. Investig Opthalmology Vis Sci. 2013;54:TFOS98. 49. Seyeddain O, Riha W, Hohensinn M. Refractive surgical correction of presbyopia with the AcuFocus small aperture corneal inlay: two-year follow-up. J Refract Surg. 2010;26:707–15. 50. Dexl A, Jell G, Strohmaier C, et al. Long-term outcomes after monocular corneal inlay implantation for the surgical compensation of presbyopia. J Cataract Refract Surg. 2015;41(3):566–75. 51. Tomita M, Kanamori T, Waring G. Simultaneous corneal inlay implantation and laser in situ keratomileusis for presbyopia in patients with hyperopia, myopia, or emmetropia: Six-month results. J Cataract Refract Surg. 2012;38(3):495–506. 52. Tomita M, Kanamori T, Waring G, et al. Small-aperture corneal inlay implantation to treat presbyopia after laser in situ keratomileusis. J Cataract Refract Surg. 2013;39(6):898–905. 53. Yilmaz Ö, Bayraktar S, Agca A, et al. Intracorneal inlay for the surgical correction of presbyopia. J Cataract Refract Surg. 2008;34(7):1921–7. 54. Yılmaz Ö, Alagöz N, Pekel G, et al. Intracorneal inlay to correct presbyopia: Long-term results. J Cataract Refract Surg. 2011;37(7):1275–81. 55. Visioneering Technology I. NaturalVue Multifocal Lens Specifications – Visioneering Technologies, Inc. Nat Multifocal Lens Specif 2018:1. 56. Sankaridurg P. Contact lenses to slow progression of myopia. Clin Exp Optom. 2017;100(5):432-7. 57. Cooper J, OʼConnor B, Watanabe R, Fuerst R, Berger S, Eisenberg N, Dillehay SM. Case series analysis of myopic progression control with a unique extended depth of focus multifocal contact lens. Eye Contact Lens. 2018;44:e16–24. 58. Tilia D, Bakaraju RC, Chung J, et al. Short-term visual performance of novel extended depth-of-focus contact lenses. Optom Vis Sci. 2016;93:435-44. 59. Bakaraju RC, Ehrmann K, Ho A. Extended depth of focus contact lenses vs. two commercial multifocals: Part 1. Optical performance evaluation via computed through-focus retinal image quality metrics. J Optom. 2018;11:10–20. 60. Bakaraju RC, Tilia D, Sha J, Diec J, Chung J, Kho D, Delaney S, Munro A, Thomas V. Extended depth of focus contact lenses vs. two commercial multifocals: Part 2. Visual performance after 1 week of lens wear. J Optom 2018;11:21–32. 61. Tilia D, Munroa A, Chunga J, Shaa J, Delaney S, Khoa D, Thomas V, Ehrmanna K, Bakarajua RC. Short-term comparison between extended depth-of-focus prototype contact lenses and a commercially-available center-near multifocal. J Optom. 2017;10:14-25. 62. Sha J, Tilia D, Kho D, Diec J, Thomas V, Bakaraju RC. Comparison of extended depth-of-focus prototype contact lenses With the 1-Day ACUVUE MOIST MULTIFOCAL after one week of wear. Eye Contact Lens. 2018;44:S157–63. 63. Sha J, Tilia D, Diec J, Fedtke C, Jong M, Thomas V, Bakaraju RC. Visual performance of myopia control soft contact lenses in non-presbyopic myopes. 2018;10:75–86. 64. Holden B, Sankaridurg P, Smith E, Aller T, Jong M, He M. Myopia, an underrated global challenge to vision: where the current data takes us on myopia control. Eye (Lond). 2014;28:142–6. 65. Huang J, Hung L-F, Ramamirtham R, Blasdel TL, Humbird TL, Bockhorst KH, Smith EL 3rd. Effects of form deprivation on peripheral refractions and ocular shape in infant rhesus monkeys (Macaca mulatta). Invest Ophthalmol Vis Sci 2009;50:4033-44. 66. Huang J, Hung L-F, Smith EL 3rd. Effects of foveal ablation on the pattern of peripheral refractive errors in normal and form-deprived infant rhesus monkeys (Macaca mulatta). Invest Ophthalmol Vis Sci 2011;52:6428-34. 67. Smith EL 3rd, Hung L-F, Huang J, Arumugam B. Effects of local myopic defocus on refractive development in monkeys. Optom Vis Sci. 2013;90:1176-86. 68. Smith EL 3rd, Hung L-F, Huang J, Blasdel TL, Humbird TL, Bockhorst KH. Effects of optical defocus on refractive development in monkeys: evidence for local, regionally selective mechanisms. Invest Ophthalmol Vis Sci. 2010;51:3864–73. 69. Zhu X, McBrien NA, Smith EL 3rd, Troilo D, Wallman J. Eyes in various species can shorten to compensate for myopic defocus. Invest Ophthalmol Vis Sci. 2013;54:2634–44. 70. Hung L-F, Ramamirtham R, Huang J, Qiao-Grider Y, Smith EL 3rd. Peripheral refraction in normal infant rhesus monkeys. Invest Ophthalmol Vis Sci. 2008;49:3747–57. 71. Kee C-S, Hung L-F, Qiao-Grider Y, Ramamirtham R, Smith EL 3rd. Astigmatism in monkeys with experimentally induced myopia or hyperopia. Optom Vis Sci 2005;82:248–60. 72. Kee C-S, Hung L-F, Qiao-Grider Y, Ramamirtham R, Winawer J, Wallman J, Smith EL 3rd. Temporal constraints on experimental emmetropization in infant monkeys. Invest Ophthalmol Vis Sci. 2007;48:957–62. 73. Qiao-Grider Y, Hung L-F, Kee C, Ramamirtham R, Smith EL 3rd. Recovery from form-deprivation myopia in rhesus monkeys. Invest Ophthalmol Vis Sci. 2004;45:3361–72. 74. Smith E, Campbell M, Irving E. Does peripheral retinal input explain the promising myopia control effects of corneal reshaping therapy (CRT or ortho-K) & multifocal soft contact lenses? Ophthalmic Physiol Opt. 2013;33:379-84. 75. Smith E, Huang J, Hung L, et al. Hemiretinal form deprivation: evidence for local control of eye growth and refractive development in infant monkeys. Invest Ophthalmol Vis Sci. 2009;50:5057-69. 76. Smith E, Hung L-F, Arumugam B, Huang J. Negative lens-induced myopia in infant monkeys: effects of high ambient lighting. Invest Ophthalmol Vis Sci. 2013;54:2959–69. 77. Smith E, Hung L-F, Huang J. Protective effects of high ambient lighting on the development of form-deprivation myopia in rhesus monkeys. Invest Ophthalmol Vis Sci. 2012;53:421-8. 78. Cooper J. Not focusing on myopia is shortsighted. J Pediatr Ophthalmol Strabismus. 2018;55:353-4. 79. PEDIG Study Group. Progressive-Addition Lenses versus Single-Vision Lenses for Slowing Progression of Myopia in Children with High Accommodative Lag and Near Esophoria. Invest Ophthalmol Vis Sci. 2011;52:2749–57. 80. Saw S, Gazzard G, Shih-Yen E, Chua W. Myopia and associated pathological complications. Ophthalmic Physiol Opt. 2005;25:381-91. 81. Saw S, Matsumura S, Hoang Q. Prevention of myopia and myopic pathology. Invest Ophthalmol Vis Sci. 2019;60:488-99. |

