 |
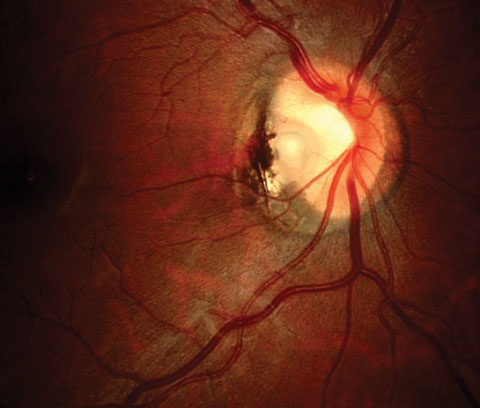
| In this study, patients diagnosed with optic disc pit exhibited at a higher mean age and a greater prevalence of visual symptoms upon their initial presentation at the clinic, compared with patients diagnosed with optic disc coloboma. Photo: Andrew Gurwood, OD. Click images to enlarge. |
OCT has revealed that retinoschisis-like retinal separations occur frequently during the development of serous macular detachments in eyes with congenital optic disc pit. In eyes with optic disc coloboma, similar serous macular detachments with retinoschisis-like separations have been reported. In terms of vision, patients with optic disc pits and colobomas typically exhibit excellent vision, unless further complicated by retinal schisis (splitting) and serous macular detachment.
A recent small study compared and reported the baseline OCT findings in eyes with optic disc pit and optic disc coloboma maculopathy to provide a plausible theory for its development in these cases. The researchers observed greater prevalence of maculopathy, presence of retinoschisis and serous macular detachment and continuation of retinoschisis but not serous macular detachment with the optic disc were eyes with optic disc pit, whereas eyes with optic disc coloboma exhibited a lower prevalence of maculopathy, presence of serous macular detachment without retinoschisis outside the coloboma and communication of the serous macular detachment with the optic disc coloboma.
Fundus examination revealed 11 eyes of 11 patients with optic disc pit and 14 eyes of 9 patients with optic disc coloboma, respectively. On OCT, maculopathy was observed more frequently in optic disc pit (n = 10) than in optic disc coloboma (n = 4) cases. In both clinical entities, hyperreflective foci were observed in the serous macular detachment. Notably, patients diagnosed with optic disc pit exhibited a higher mean age and a greater prevalence of visual symptoms upon their initial presentation at the clinic, compared with patients diagnosed with optic disc coloboma.
“One potential factor contributing to the observed phenomenon in the current study is the comparatively earlier onset of optic disc coloboma cases, which may result in the gradual development of maculopathy over a period of time,” the researchers wrote in their paper. “The structure of the optic disc’s margin may also serve as a potential barrier against the development of maculopathy during the initial phases.”
Retinoschisis outside the coloboma without retinal detachment is uncommon in eyes with optic disc coloboma, the researchers state, “except for eyes with long-standing retinal detachment, in which the retinal detachment itself causes degenerative splitting of the inner retinal layers,” they added. “This best explains the glaring differences between optic disc pit and optic disc coloboma maculopathy characteristics noted in our study.”
The OCT characteristics and visual symptoms in optic disc pits and colobomas may serve as a guide when considering intervention in such cases. The researchers recommend that clinicians take a step-by-step approach when considering interventional treatment for each type of case based on the presence of maculopathy, progression of maculopathy and recent onset of visual symptoms.
“We stress the importance of analyzing the entire cube scan at the optic disc margin in order to evaluate the communication between the subretinal fluid and optic disc pit or optic disc coloboma when planning intervention in these cases,” the authors wrote. “Moreover, the role of swept-source OCT imaging cannot be overlooked in such clinical settings, particularly in eyes with optic disc coloboma.”
Prabhu V, Mangla R, Acharya I, et al. Evaluation of baseline optic disc pit and optic disc coloboma maculopathy features by spectral domain optical coherence tomography. Int J Retina Vitreous. 2023;9(1):46. |

