 |
A 23-year-old white female presented for an evaluation of blurred vision in both eyes. She reported the right eye had been worse for over six months, and she felt like there was a “dead spot” in her central vision. The left eye had been getting worse over the past one month. She reported having been very near-sighted all her life and started wearing glasses at a very young age.
Her past medical history was significant for Crohn’s disease, which was diagnosed at age 14, that she treats with Entyvio (vedolizumab, Millennium Pharmaceuticals) IV once a month. She reported having a recent flare-up.
On exam, her best-corrected visual acuity measured 20/400 OD with eccentric viewing and 20/70 OS. Her prescription measured -8.00D with 2.00D of astigmatism in each eye. Extraocular motility testing was normal. Confrontation visual fields were full-to-careful finger counting OU.
Amsler grid showed a central scotoma in both eyes but was very dense in the right eye. Her pupils were equally round and reactive to light; there was no afferent pupillary defect. The anterior segment examination was unremarkable. Tensions by applanation were 12mm Hg OD and 11mm Hg OS.
The dilated fundus examination revealed a clear vitreous in both eyes. The optic nerve was slightly tilted but had good rim coloration and perfusion. There was situs inversus of both optic nerves. She had a myopic-appearing fundus, and other significant changes were noted (Figure 1). An OCT was performed and is available for review (Figure 2).
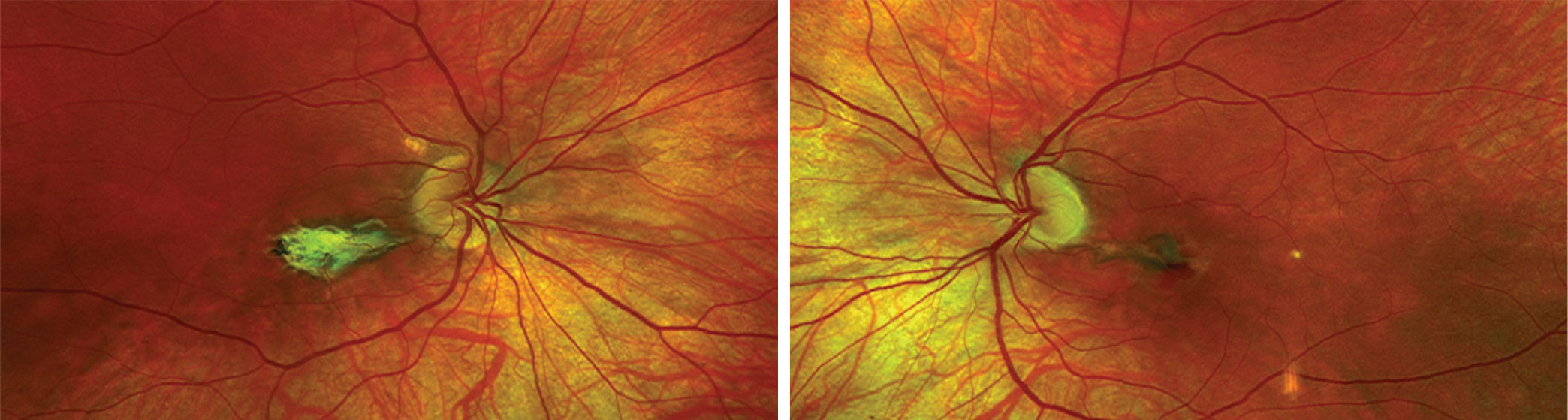 |
| Fig. 1. This is the widefield fundus photo of the right (at left) and left eyes of our patient. What does the change in the macula represent? Click image to enlarge. |
Take the Retina Quiz
1. What is the patient’s underlying condition?
a. Degenerative myopia
b. Ocular histoplasmosis
c. Pseudoxanthoma elasticum (PXE)
d. Punctate inner choroidopathy (PIC)
2. How would you characterize the macula in her right eye?
a. Fibrotic disciform scar
b. Active choroidal neovascularization (CNV)
c. Fuchs’ spot
d. Angioid streak
3. How would you characterize the macula in the left eye?
a. Fibrotic disciform scar
b. Active CNV
c. Fuchs’ spot
d. Angioid streak
4. How should our patient be treated or managed?
a. Observation in both eyes
b. Intravitreal steroid in one or both eyes
c. Treatment with anti-VEGF injection in both eyes
d. Treatment with anti-VEGF in left eye
5. What is the patient’s likely visual outcome at this point?
a. Good vision in the left eye is likely
b. Poor in both eyes—worse than 20/200
c. Too early to determine
d. Could go either way
For answers, see below.
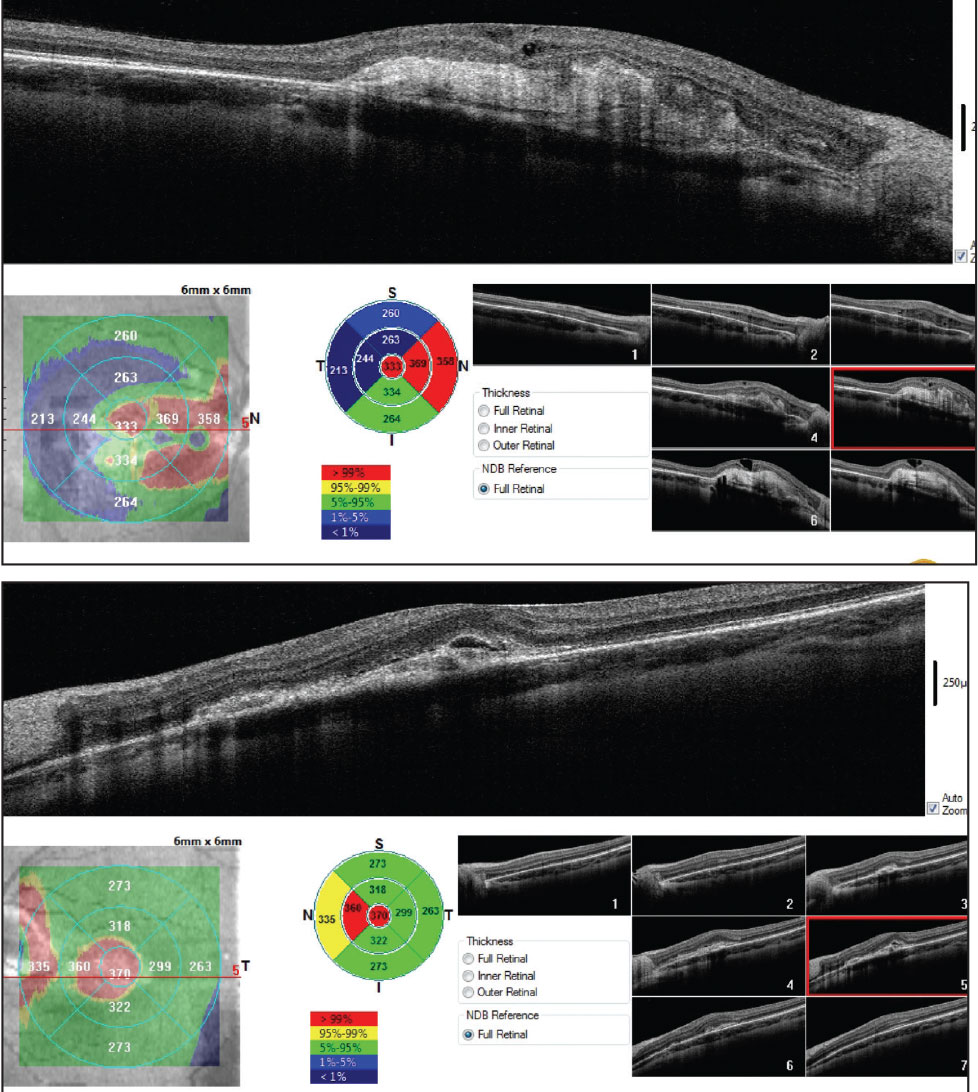 |
| Fig. 2. This is the OCT through the macula of the right (on top) and left eyes. Click image to enlarge. |
Discussion
In the right eye, there is a fibrotic disciform scar forming that involves the patient’s fovea and thus explains why she is 20/400 eccentrically viewing. In the left eye, there is a gray-green pattern that is visible between the optic nerve and macula. In addition, there is also a subretinal hemorrhage present on the temporal side near the fovea.
Unfortunately, our patient has bilateral CNV. The right eye is inactive and in the process of forming a fibrotic, disciform scar, but the CNV in the left is more recent. Subretinal fluid can be seen on the OCT in addition to a broad, dense reflective area anterior to the retinal pigmented epithelium (RPE), which likely represents the CNV. The CNV is likely above, or anterior to, the RPE because we were able to visualize the gray-green pattern on our clinical exam. Categorically, this represents a type 2 CNV, instead of a type 1, which is located below the RPE.
So, what is the underlying etiology for the CNV? It’s not a straightforward, easy answer. She has significant myopia and clearly has myopic degenerative changes, so myopia could be a possibility. CNV associated with degenerative myopia is common and represents one of the top CNV causes, behind macular degeneration and ocular histoplasmosis.
Could this be from histoplasmosis? She does have some focal depigment spots in the posterior pole of both eyes that resemble “histo” spots. But there aren’t that many spots, and there are none in the periphery. What’s more, there isn’t any pigment hypertrophy surrounding the spots, which is characteristic of histo spots, nor is there any peripapillary atrophy around the optic nerve. These are all classic features of ocular histoplasmosis. However, our patient is from Minnesota and, though maybe not typically considered to be part of the “Histo-belt” (Ohio and Mississippi River Valley), histoplasmosis is common in areas of Minnesota.1
Coupled with Myopia
More likely, our patient has PIC, an inflammatory disease of the choroid and RPE that affects young myopic women. Over 90% affected are female, and 85% have myopia with a median age of 30 (range 15 to 55).2-4 It is characterized by multifocal, well-circumscribed, yellow-white choroidal lesions in the posterior pole in the absence of anterior segment inflammation and vitreous cells.
These yellow-white lesions are present in our patient. In the right eye, a lesion can be seen adjacent to the optic nerve, and in the left eye, two are clearly present: one temporal to the macula and the other one along the inferior arcade and even a possible third one just above the macula.
Patients with PIC may be completely asymptomatic unless the lesions affect the fovea. If this occurs, patients can have blurred vision, scotoma, metamorphopsia and even photopsia. CNV can develop in up to 70% of patients with PIC, in which case severe visual loss may occur unless it is treated.2,4
The exact cause of PIC is poorly understood. One thought is that it results from an autoimmune response to previous viral infections coupled with a genetic predisposition or family history. Environmental triggers, such as stress, may also play a role.3
For many patients with PIC, visual function is unaffected, and there is no need for treatment. For patients who develop active lesions in the macula, corticosteroids may be effective, as this is considered to be an inflammatory disease, and steroids have shown a beneficial effect. For patients who develop CNV, anti-VEGF is the treatment of choice, either alone or in combination with oral corticosteroids.
To Sum Up
In our patient, the CNV in the right eye was inactive, and because she is already forming a fibrotic scar, there would be no benefit of treating it. But the CNV in the left eye is active and, for that reason, she was referred to a retina specialist where anti-VEGF therapy was initiated. She continues to be followed on a monthly basis by the retina specialist.
Retina Quiz Answers
1) d; 2) a; 3) b; 4) d; 5) a.
Dr. Dillinger practices at Horizon EyeCare in Owatonna, MN. He has no financial interests to disclose.
Dr. Dunbar is the director of optometric services and optometry residency supervisor at the Bascom Palmer Eye Institute at the University of Miami. He is a founding member of the Optometric Glaucoma Society and the Optometric Retina Society. Dr. Dunbar is a consultant for Carl Zeiss Meditec, Allergan, Regeneron and Genentech.
| 1. Armstrong PA, Jackson BR, Haselow D, et al. Multistate epidemiology of histoplasmosis, United States, 2011-2014. Emerg Infect Dis. 2018;24(3):425-31. 2. Essex RW, Wong J, Fraser-Bell S, et al. Punctate inner choroidopathy: clinical features and outcomes. Arch Ophthalmol. 2010;128(8):982-7. 3. Jampol LM, Becker KG. White spot syndromes of the retina: a hypothesis based on the common genetic hypothesis of autoimmune/inflammatory disease. Am J Ophthalmol. 2003;135:376-9. 4. Campos J, Campos A, Mendes S, et al. Punctate inner choroidopathy: a systematic review. Med Hypothesis Discov Innov Ophthalmol. 2014;3(3):76-82. |

