 |
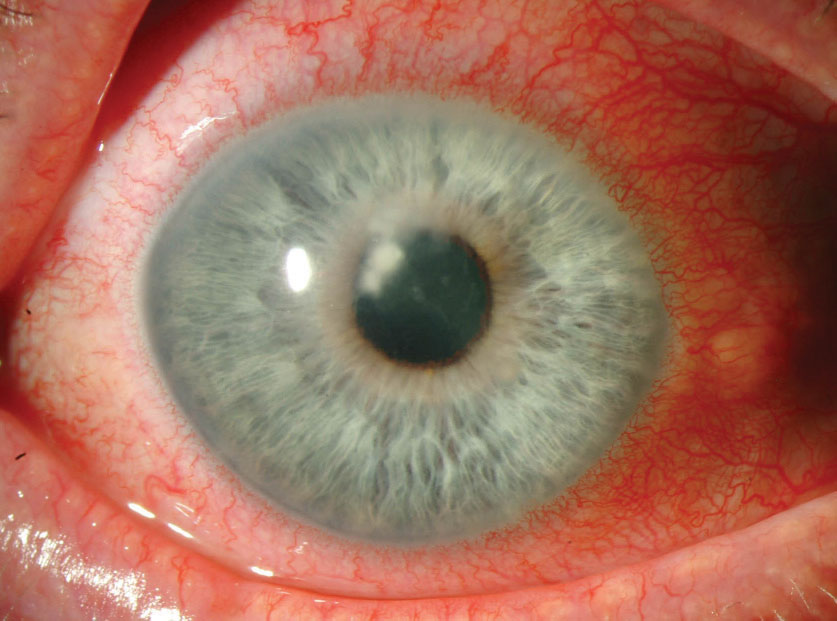
Astigmatism and scar size each mediated 23% of the effect of crosslinking on BSCVA. Photo: Christine W. Sindt, OD. Click image to enlarge. |
Crosslinking-assisted infection reduction, abbreviated as CLAIR, is a randomized, outcome-masked clinical trial that evaluates the benefit of adjuvant corneal crosslinking in moderate to severe bacterial keratitis. Studies have shown that photochemically-activated riboflavin may be effective against some ocular pathogens.1,2 In fact, because the photochemical reaction between UV light and riboflavin kills pathogens, crosslinking is safe to perform outside the operating room at the slit lamp.3 However, this novel approach isn’t approved in the United States yet.
Crosslinking is currently being assessed for its possible use against infectious keratitis and as an adjunctive therapy in fungal keratitis.4,5 So far, it’s proved less useful in cases of fungal keratitis. Researchers believe this may be due to the fact that fungal infections tend to penetrate deeper into the cornea than most bacteria.4 In the CLAIR study, however, the researchers discovered another important finding: “Patients with filamentous fungal corneal ulcers who underwent adjunctive crosslinking in addition to topical antifungal treatment had worse visual acuity outcomes than those treated with antifungal alone.”5
“It’s been well established that corneal crosslinking can cause corneal haze and topographic changes in patients with keratoconus,” the CLAIR researchers wrote in a secondary analysis of the trial that explored whether astigmatism or corneal scarring mediates reduced visual acuity among fungal keratitis patients who received crosslinking. “The reason for [poorer visual outcomes with adjunctive crosslinking] is unclear but could be related to increased irregular astigmatism, scar size or scar density after crosslinking.”
In their paper, they reported this prespecified exploratory outcome of the CLAIR trial (NCT02570321). Consecutive patients who presented with moderate vision loss from a smear-positive fungal ulcer at Aravind Eye Hospital in Madurai, India, were randomized to one of four treatment combinations with an adaptive randomization protocol. A total of 111 patients were randomized to the following treatment arms: topical natamycin 5%, topical natamycin 5% + CXL, topical amphotericin B 0.15% and topical amphotericin 0.15% + CXL. BCVA, contact lens over-refraction and scar size and depth were measured in a masked study by an ophthalmologist using a standardized protocol at three months. Patients underwent Pentacam Scheimpflug imaging at three months as well.
The researchers reported that 99 of 111 patients whose data was available at three months had a mean BSCVA of 0.82 logMAR (Snellen equivalent 20/132). They found that the patients’ three-month infiltrate and/or scar size, depth and densitometry were statistically significant predictors of three-month BSCVA. “Astigmatism seemed to mediate 23% of the effect of crosslinking on BSCVA, whereas scar size mediated 23%, scar depth 17% and densitometry 7%,” they reported.6
Together, these factors mediated approximately 47% of the crosslinking effect on visual acuity in cases of fungal keratitis in the study. “Normal corneal tissue is transparent with minimal light scatter,” they wrote. “However, during acute infectious keratitis, inflammatory cells invade the corneal stroma, disrupting the regular arrangement of collagen fibrils and causing an increase in corneal light scatter. The mechanism for increased scarring after crosslinking in fungal keratitis is unclear and may involve altered leukocyte density or trafficking during wound healing or reduced keratocyte and basal nerve plexus density.”
They noted that densitometry poorly correlated with other corneal scarring measures; they believe this may mean that densitometry measures different aspects of corneal health. “Corneal densitometry may be an additional indicator of corneal health beyond slit lamp examination and may even aid in distinguishing reduced visual acuity from corneal pathology from that of the optic nerve or retina,” they wrote. “A previous study of densitometry after crosslinking in keratoconus showed that densitometry values increased by approximately 2 GSU on average but returned to baseline values by 12 months post-crosslinking.”
Importantly, their mediator analysis demonstrated that 23% of the crosslinking effect on visual acuity was due to astigmatism. “Those randomized to crosslinking did indeed have almost 5D higher astigmatism on average, although this wasn’t a statistically significant finding. Studies of Pentacam in patients with keratoconus have shown that crosslinking generally causes a flattening and normalization of the corneal shape compared with pre-crosslinking measurements. The fact that CTL-Rx improved visual acuity in our study is supportive of the notion that astigmatism after corneal infection plays a significant role in reducing BSCVA. However, those randomized to crosslinking had almost five lines’ worse visual acuity with CTL-Rx on average, suggesting that visually significant scarring is still the most important factor.”
They concluded that corneal scarring and astigmatism were mediators of worse visual acuity in patients with fungal keratitis who received crosslinking. Additionally, “corneal densitometry may be a helpful cornea-specific variable for clinicians and researchers in determining the effect of corneal scarring on visual acuity in specific patients and as an objective study outcome.”
1. Martins SA, Combs JC, Noguera G, et al. Antimicrobial efficacy of riboflavin/UVA combination (365 nm) in vitro for bacterial and fungal isolates: a potential new treatment for infectious keratitis. Invest Ophthalmol Vis Sci. 2008;49(8):3402-8. 2. Wollensak G, Spoerl E, Reber F, Seiler T. Keratocyte cytotoxicity of riboflavin/UVA-treatment in vitro. Eye (Lond). 2004;18(7):718-22. 3. Hafezi F, Richoz O, Torres-Netto EA, et al. Corneal cross-linking at the slit lamp. J Refract Surg. 2021;37(2):78-82. 4. Deshmukh R. Commentary: PACK-CXL in fungal keratitis. Indian J Ophthalmol. 2019;67(10):1701-2. 5. Prajna NV, Radhakrishnan N, Lalitha P, et al. Cross-linking-assisted infection reduction: a randomized clinical trial evaluating the effect of adjuvant cross-linking on outcomes in fungal keratitis. Ophthalmology. 2020;127:159-66. 6. Prajna NV, Radhakrishnan N, Lalitha P, et al. Mediators of the effect of corneal cross-linking on visual acuity for fungal ulcers: a prespecified secondary analysis from the cross-linking-assisted infection reduction trial. Cornea. 2022;00:1-5. |

