Researchers from Australia wanted to know how lack of oxygen affects the different areas of the ocular surface—specifically, the cornea. Contact lenses can induce hypoxia and have been used in previous studies to impair oxygen delivery to the cornea, but this can create variations in hypoxia magnitude across the surface because of regional differences in contact lens thickness, fluid reservoir thickness in scleral lenses and extent of tear exchange.
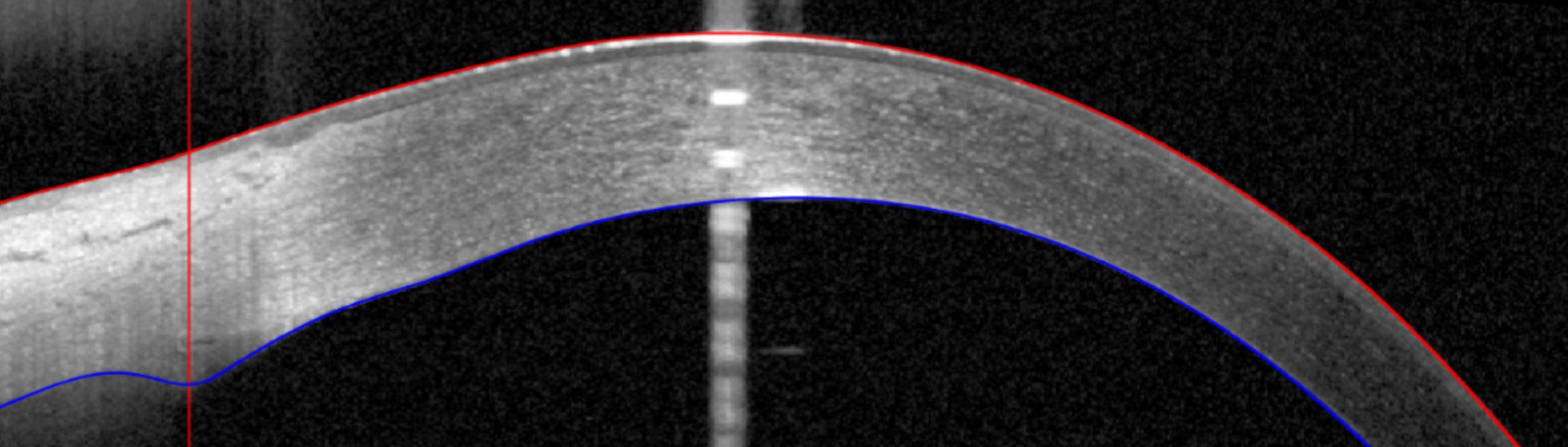 |
| :Images were captured more peripherally in the limbal region, and greater peripheral swelling could be related to increased conjunctival/scleral blood flow or thickness, which have been documented following overnight eyelid closure. Photo: Iqbal et al. Ophthalmic Physiol Opt. 2024;00:1-6. Click image to enlarge. |
Instead, the current study induced short-term, unilateral eyelid closure to induce hypoxia without contact lens wear. The left eye of 10 healthy adult corneas were patched for 30 minutes using a folded eye pad. OCT images—which captured the limbal and central corneal regions simultaneously—were obtained before patching, immediately after eye opening and at one, two, five, six, nine, 10, 14 and 15 minute marks after eyelid opening. Edema was measured from the limbus (scleral spur) to the central cornea (thinnest corneal location) along the horizontal meridian.
After 30 minutes of this eyelid closure, a greater amount of limbal edema (55%) was seen when compared with the central cornea; this was 3.84% at the nasal limbus and 2.48% at the central cornea. However, both the central and limbal edema recovered rapidly (within one to two minutes) after eyelid opening. No significant differences in the rate of corneal recovery were seen between corneal locations.
Upon discussion, the study authors elaborate that these findings are contradictory to previous findings, which found greater edema levels in the central, rather than peripheral cornea. They explain that this difference likely is due to methodological difference in image capturing across studies following the removal of the hypoxic stimulus. As an example, they explain that two previous investigations used optical pachymetry, which may result in underestimation of edema for some corneal locations, since corneal thinning occurs within one to two minutes after hypoxic stimulus removal—with pachymetry taking longer than that. A different explanation may be because of corneal measurement locations. The current study captured limbal measurements at the scleral spur using OCT, while previous reports were confined to mid-peripheral or peripheral corneal locations.
They also note that rapid corneal thinning and overshoot (thinning beyond the baseline corneal thickness) was observed 1.5 minutes after eyelid opening, which remained stable throughout the 14.5 minute recovery period. Overshoot has been reported in prior investigations as well and is hypothesized to be to be modified by hydration factors like tear evaporation rate, endothelial ion pump function and alterations in tear osmolarity from low humidity.
Looking forward, the authors relay that “further research is required to examine the impact of limbal oxygen supply and the potential peripheral clamping effect upon the regional corneal response to hypoxia.”
Iqbal A, Fisher D, Alonso-Caneiro D, Collins MJ, Vincent SJ. The central and peripheral corneal response to short-term hypoxia. Ophthalmic Physiol Opt. 2024;00:1-6. |

