 |
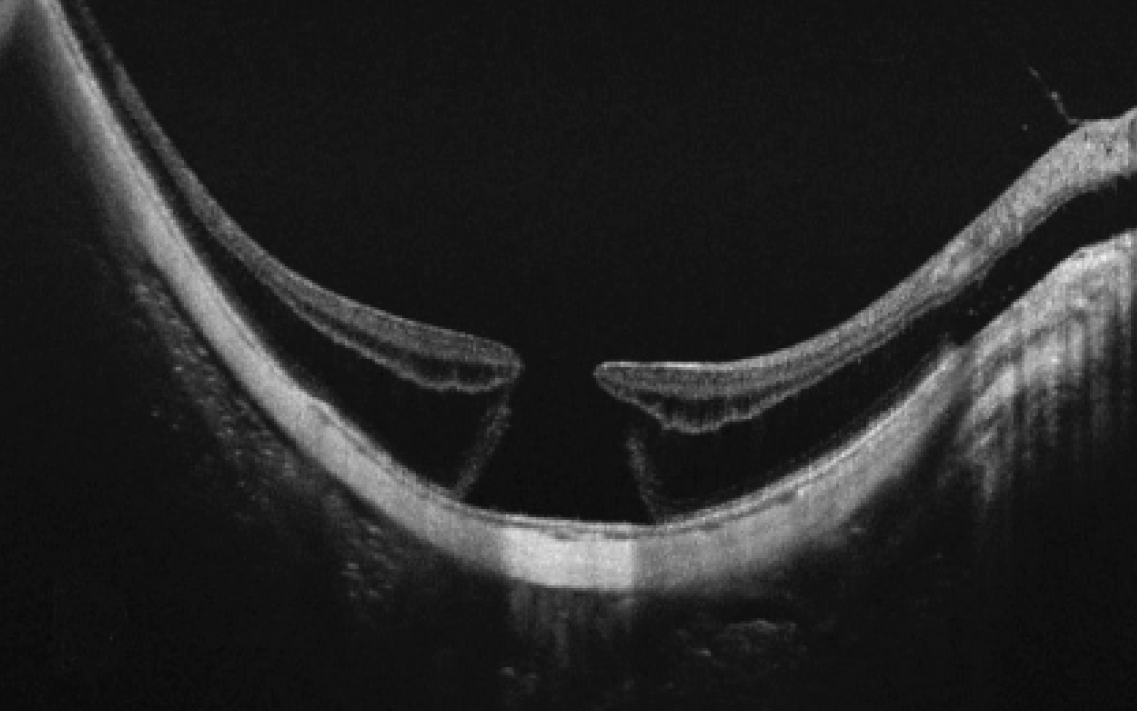
| Posterior sclera reinforcement is recommended for grades 1 and 2 MTM, while in grade 3 and pre-advanced stage MTM, performing posterior sclera reinforcement is advised, with vitreoretinal surgery or macular buckling suggested if the patient loses two or more lines of BCVA in three months. Photo: Feng JJ. Clin. Med. 2022. Click image to enlarge. |
With a greater increase in prevalence of high myopia, optometrists and ophthalmologists need to be more vigilant for the ensuing retinal vulnerabilities such patients experience. Myopic traction maculopathy (MTM), when advanced in stage, can cause irreversible visual impairment. As such, researchers of one new study sought to learn more about the potential clinical features of foveal detachment, full-thickness macular hole and macular hole retinal detachment in advanced cases of MTM.
The study—including 314 eyes of 198 patients—retrospectively observed cases of retinoschisis from Beijing Tongren Hospital. Sex, age and axial length were recorded, and OCT was used to evaluate fundus characteristics. Vitreoretinal interface condition was described through epiretinal membranes (ERMs), vitreoretinal traction and paravascular abnormalities. Retinal condition was revealed through different retinoschisis layers (including inner, middle and outer) and by location with a range of outer retinoschisis. Finally, five patterns of scleral shape, including dome-shaped, sloped toward optic nerve, symmetrical or asymmetrical around fovea and irregular were assessed to show retina-sclera condition.
After analysis, 76 eyes exhibited foveal detachment, six eyes exhibited full-thickness macular hole and seven showed macular hole retinal detachment, with an average age of 60±12.3 years. Advanced eyes were older, had higher ERM rates, paravascular abnormalities, middle and outer retinoschisis and possessed more of those with irregular sclera shape. What’s more, the advanced stage correlated with more retinoschisis layers and a higher grade of outer retinoschisis. Upon multivariate analysis, ERMs, middle retinoschisis and higher graded outer retinoschisis remained associated with the advanced MTM stage.
When comparing their results to previous literature, the study authors point out that although their data indicated greater age in the advanced group than controls, it was not related to severe stage after adjusting for other factors, which is something that prior research has indicated. Instead, they offer that aging may be related with other factors, like ERMs, sclera shape and outer retinoschisis degree, but after correcting for these, aging was not considered an independent risk factor.
Furthermore, literature has found a shorter axial length to map onto eyes with myopic retinoschisis when compared with highly myopic eyes without. However, this study did not find axial length to be associated with advanced stage. The researchers propose posterior staphyloma, which challenges measuring axial length, may have a more prominent effect on MTM development through its height, as might scleral wall shape, over axial elongation.
The vitreoretinal interface was described by ERMs, vitreoretinal traction and paravascular abnormalities. The authors saw greater correlation of ERMs with MTM advanced stage than the other two characteristics, prompting them to address that “ERMs might provide more vital traction on the macular lesion. In addition, the vitreoretinal traction could be less visible on OCT.”
The observed irregular sclera shapes seen with advanced stage were hypothesized to be indicative of aging, axial elongation and disease evolution, as it was not significantly associated after multivariate analysis.
Based on their findings, the authors posit some clinical suggestions for management. For one, they believe inner and middle retinoschisis without outer schisis should be considered as grade 1, as these cases were rare in the data and did not display advanced stage. Second, partial to outer retinoschisis, classified as S1 to S3, are recommended to be regarded as grade 2. In advanced stage, or stage 3, they suggest “regarding middle retinoschisis and ERMs as plus lesions to underline the associated characteristics of the advanced stage.” MTM eyes with foveal detachment, full-thickness macular hole and macular hole retinal detachment are considered grades 4, 5 and 6, respectively. As all three grades are considered advanced, the authors add that “vitreoretinal surgery or macular buckling is necessary” in this stage, “besides, posterior reinforcement is recommended for patients undergoing vitrectomy to improve postoperative visual acuity and prevent disease progression.”
Tian J, Lin C, Fang Y, et al. Multimodal analysis on clinical characteristics of the advanced stage in myopia traction maculopathy. Ophthalmol Ther. July 8, 2023. [Epub ahead of print]. |

