 |  |
We try our best to protect the ocular surface from the onslaught of forces that can disrupt it, but sometimes the superficial cornea just isn’t amenable to repair. If so, superficial keratectomy (SK) can greatly improve visual quality. This minimally invasive procedure removes the epithelium down to Bowman’s membrane, then uses a corneal hoe or beaver blade to remove deposits, opacities or diseased tissue. A diamond burr polishes Bowman’s, ensuring a smooth surface for new corneal epithelial cells to migrate over and proliferate.
The overall goal is to create a more regular corneal surface by allowing new epithelial growth to proceed uniformly.
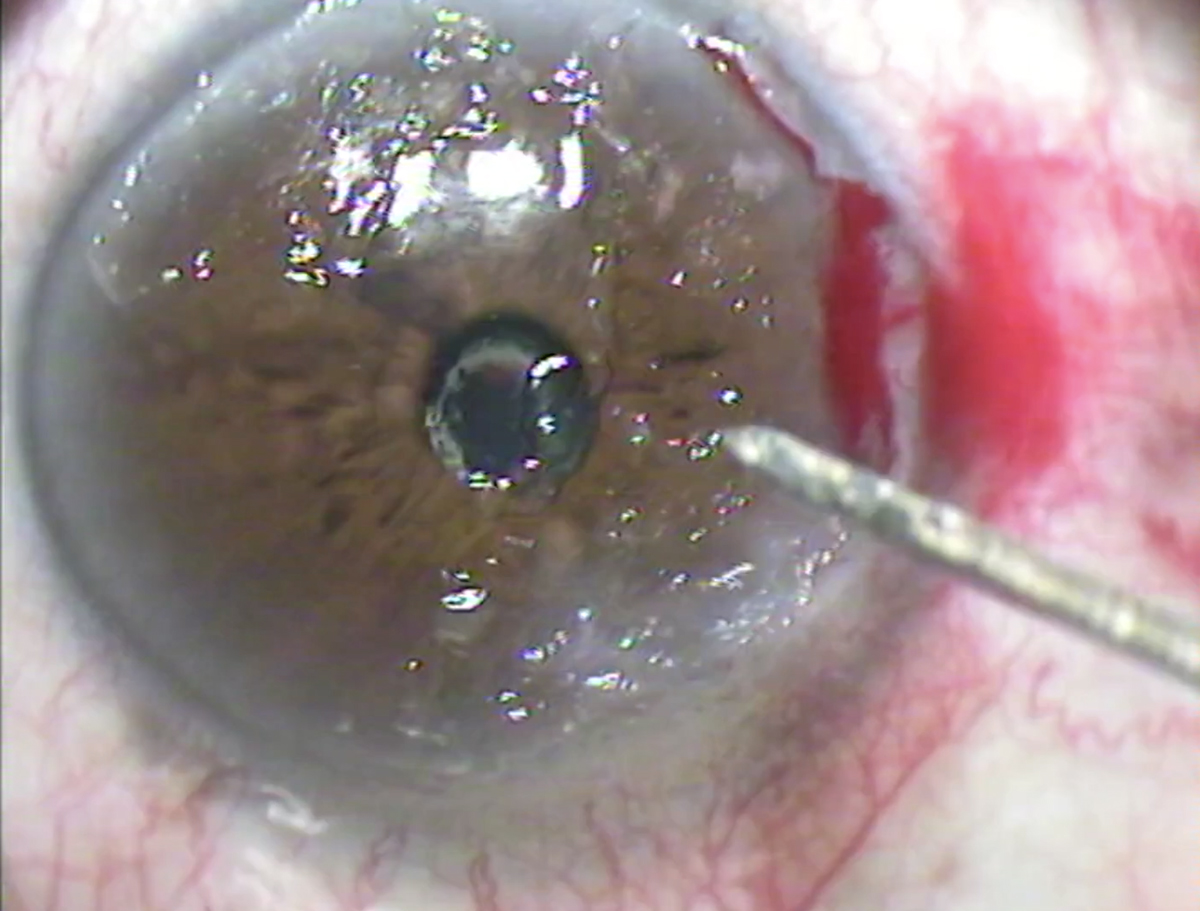 |
| Superficial keratectomy involves the manual removal of superficial corneal scar tissue. Photo: Dell Laser Consultants. Click image to enlarge. |
Since many cases can be comanaged by optometrists, it’s important for ODs to be knowledgeable about SK’s indications and well-versed in the procedure to tackle any post-op complications. Diseases treated with SK include:
• Salzmann’s nodular degeneration, in which superficial, elevated, blue-white lesions appear in Bowman’s immediately behind the epithelial basement membrane. The pathogenesis is unclear, but these typically occur after chronic inflammation to the ocular surface, which can be brought on by longstanding dry eye disease.
• Anterior basement membrane dystrophy, an inherited disorder and the most common corneal dystrophy, occurs when areas of the basement membrane thicken and protrude, causing raised areas and irregularities. It’s typically diagnosed from significant negative fluorescein staining on the epithelium. Severe cases can induce irregular astigmatism, decreasing quality of vision.
• Recurrent erosion, which occurs from poor hemidesmosomal connection between epithelial cells and their basement membrane. This causes epithelium to slough off in specific areas, which can be quite painful when located close to corneal nerves.
• Pterygium, or abnormal scleral tissue growth that extends over the cornea. This is a protective response usually seen from increased UV light exposure. When significant, it can cause extensive irregular astigmatism.
• Band keratopathy, due to calcium salt deposits in Bowman’s, is usually not visually significant but can be removed if cosmetically unappealing.
Since mild forms of these diseases are managed with various dry eye treatments and topical steroids, SK is typically reserved for more moderate-to-severe cases. However, it may be considered for milder ones that cause only minor irregularities if there is a need for detailed refractive measurements (e.g., prior to cataract extraction surgery).
Postoperative Care
Immediately following the procedure, a bandage contact lens is placed on the eye, sometimes with an amniotic membrane under the lens to aid re-epithelialization. The patient is often prescribed a topical antibiotic, steroid and artificial tear. Discomfort the night after the procedure, as well as the next day, is common. If needed, an oral pain medication can also be prescribed. Vision is also expected the first week as the cornea re-epithelializes and slowly improves over the next few weeks.
Follow-up schedule includes a one-day post-op visit to evaluate comfort, look for signs of inflammation and confirm the bandage lens has remained centered. Next, the patient usually returns one week later to ensure the cornea has re-epithelialized. If so, the lens is removed and the antibiotic is discontinued. Lastly, the patient returns for a one-month post-op visit to ensure vision has improved and stabilized.
Keep in mind that a patient may need to undergo multiple SKs in their lifetime due to the recurrent nature of things like Salzmann’s nodules. The conditions listed can worsen with chronic dry eye, which is more prevalent with age. This procedure is not meant to be a “cure,” but rather a long-term maintenance of the patient’s condition. It’s important to articulate this to your patients to ensure realistic expectations.
Dr. Zimmerman is an ocular disease resident at Dell Laser Consultants in Austin, TX. He has no financial disclosures.
Dr. Cunningham is the director of optometry at Dell Laser Consultants in Austin, TX. He has no financial interests to disclose. Dr. Whitley is the director of professional relations and residency program supervisor at Virginia Eye Consultants in Norfolk, VA. He is a consultant for Alcon.

