 |  |
Historically, a dysfunctional cornea had been surgically managed with a single approach: full-thickness penetrating keratoplasty (PK). First performed in 1905, this corneal transplantation procedure is still frequently used today. It is the most successful solid organ transplantation in the body due to corneal avascularity and immune privilege.1 The 2023 Eye Bank Association of American report distributed tissue for 50,925 keratoplasties, 14,486 of which were used for PK.2
The goal of the procedure is to replace opacified or distorted tissue with clear donor tissue. This can be helpful to establish a clear visual axis, alleviate painful conditions and sometimes help treat infections. The procedure is indicated for corneal conditions that affect multiple layers of the cornea and is relatively contraindicated in patients with ocular surface disease, as this is a leading cause of transplant failure.1
Candidate selection, preoperative preparation and postoperative management are important considerations to maximize chances of success. Preoperative patient education should mention that it often takes 12 months to achieve maximal visual rehabilitation; however, there will likely be refractive error remaining. Postoperative patient education is just as important, which we will discuss in extensive detail below.
 |
|
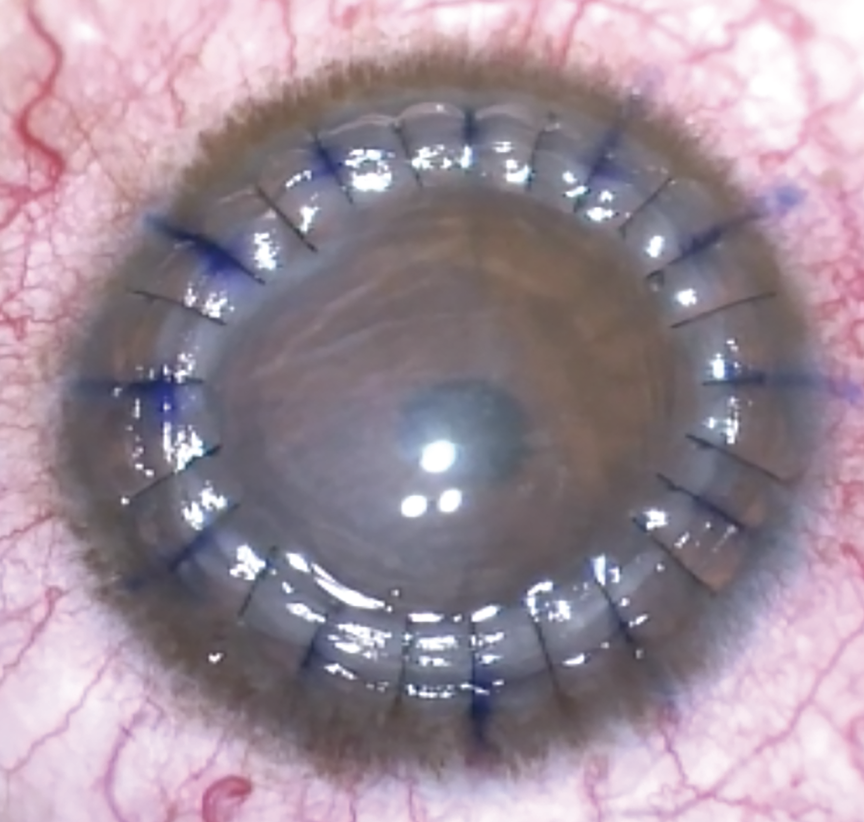
Post-op following PK is crucial, especially the first three months, to monitor for possible complications such as broken sutures or signs of graft rejections. Photo: Albert Cheung, MD. Click image to enlarge. |
Performing the Procedure
A circular cutting device known as a trephine is used to precisely cut a round corneal button of donor tissue. A similar size cut is made to the host cornea. After the host corneal button is removed, the donor button is placed and sutured into place. The nylon sutures are tied and buried on the donor side, as far from the limbus as possible. The surgeon will take care to evenly distribute suture tension, as tight sutures can lead to a flat corneal surface and resultant severe astigmatism. There are several suturing techniques used, including interrupted sutures only, running suture only, combined interrupted and running, and double running. However, there is no proven superior technique.
Post-op
Close observation is a necessity. At post-op day one, the patch and eye shield are to be removed so that topical medications can be applied. Prophylactic topical antibiotics and steroids are prescribed four times daily with a slow taper on steroids over the next few months. Topical nonsteroidal anti-inflammatories may be used in combined cataract and PK surgeries. At this initial visit, the physician must check carefully for wound leakage, treat ocular surface disease and/or epithelial defects, manage intraocular pressure complications and address pain symptoms.
Postoperative patient education is key. Light activity, avoidance of eye rubbing and wearing nighttime shield for the first week is imperative. Protective eyewear should always be worn during sporting or other activities that risk ocular trauma, and religious use of anti-rejection drops is mandatory. Patients must know the signs and symptoms of loose sutures, infection and graft rejection, which require prompt intervention to have a chance at preserving the graft.
While long-term management is extremely important, close observation over the first three months is required to monitor for any of a host of complications that can arise, especially signs of graft rejection. An episode of decreased vision, redness and light sensitivity lasting more than a few hours should raise suspicion for graft rejection. Corneal edema within the graft, anterior chamber cells/flare and circumciliary injection may be the earliest presenting signs of rejection. Epithelial rejection lines, subepithelial infiltrates, stromal haze, keratic precipitates and endothelial rejection lines may also occur.
Risk factors for rejection include previous graft failure, large grafts, young age, preoperative glaucoma, corneal neovascularization, anterior synechiae, ocular surface disease and previous herpetic infection.3 Signs of rejection are treated aggressively with topical steroids and cyclosporines; however, exercise caution in patients with a history of herpes simplex keratouveitis. Prompt referral back to the surgeon should be made as subconjunctival injections or oral steroids may be used and graft rejection can be reversed with prompt and aggressive therapy. Thankfully, PK is largely successful with approximately 95% of grafts clear at five years for low-risk eyes.4 Even without signs of rejection, patients are usually kept on one drop of topical steroids daily for life.
Many of these patients will achieve maximum visual rehabilitation only with the use of specialty contact lenses. The fitting process can start as soon as three to four months postoperatively, as long as the graft is healthy and the surgeon agrees. However, it can take much longer to fully stabilize, and suture adjustments can complicate the fitting process.
As comanaging optometrists, we are the providers concerned with long-term postoperative management. Thus, we must always remain vigilant for complications such as broken sutures or signs of graft rejection which often occurs years after the procedure.
Dr. Black graduated from Nova Southeastern College of Optometry and completed residency in ocular disease at Bascom Palmer Eye Institute. He practices at Virginia Eye Consultants in Virginia Beach. He has no financial disclosures.
1. Mannis MJ, Holland EJ. Cornea. 5th ed. Elsevier; 2021. 2. Eye Bank Association of America. Statistical Report. restoresight.org/members/publications/statistical-report. Accessed May 22, 2024. 3. Panda A, Vanathi M, Kumar A, et al. Corneal graft rejection. Surv Ophthalmol. 2006;52(4):375-96. 4. Thompson RW, Price MO, Bowers PJ, et al. Long-term graft survival after penetrating keratoplasty. Ophthalmology. 2003;110(7):1396-402. |

