 |  |
Regeneration of the corneal epithelium, crucial for ocular health, is maintained by limbal stem cells. Trauma, contact lens overwear or inflammatory issues can cause these cells to struggle, leading to limbal stem cell deficiency (LSCD). The condition can also be congenital in patients with aniridia or autoimmune disorders.
Early LSCD may be controlled with topical treatment to decrease inflammation, including topical steroids, ocular cyclosporine or amniotic membrane grafts or drops. If contact lenses are the cause, discontinuing wear or refitting in a daily option or scleral lens can help minimize further limbal stem cell damage. But once these patients progress to more severe LSCD and their vision becomes threatened by recurrent, non-healing epithelial defects, corneal scarring and melts, it is time to consider surgical options.
Procedures
Multiple approaches to limbal stem cell transplantation exist. Depending on the surgeon’s preference and the extent of LSCD damage, different techniques may be better than others. The most common option is keratolimbal allograft (KLAL), which uses allogeneic limbal tissue attached to a corneoscleral carrier from a cadaveric donor. This procedure is common for those with bilateral LSCD who may not have a related donor, or those with unilateral LSCD and the other eye is not a viable donor.1 Ideal candidates have LSCD caused by aniridia, contact lens wear and iatrogenic LSCD with minimal to no conjunctival involvement. KLAL can also help to treat mucous membrane pemphigoid and Stevens-Johnson syndrome, if they are controlled and quiet for at least a year prior to surgery.
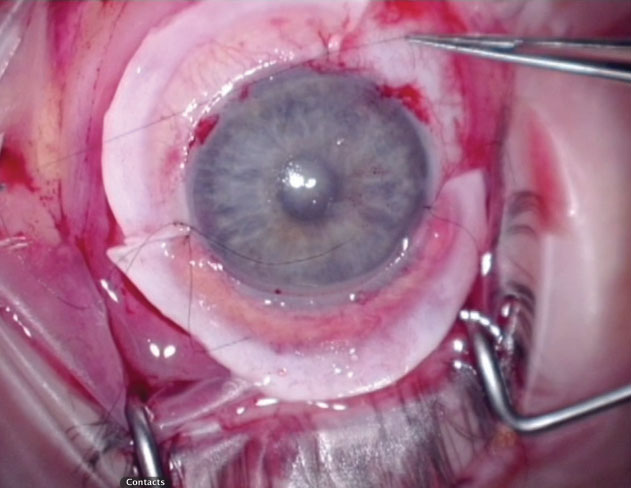 |
During the procedure, lenticules from a donor cornea are sutured along the limbus and secured with tissue glue. |
The surgical technique uses two donor corneoscleral rims that are divided into four crescents. Three of these crescents are then placed around the recipient’s cornea with the donor tissue’s anterior corneal edge overlying the recipient’s limbus. As the patient heals, the gaps between the KLAL segments fill in with repopulated healthy cells.
Post-op Management
At the time of surgery, a bandage contact lens is placed in the operative eye and maintained until the corneal epithelium is healed. Patients are prescribed topical lifitegrast or cyclosporine, a topical steroid, a fluoroquinolone and frequent use of preservative-free artificial tears. Once the bandage contact lens is removed, the antibiotic is discontinued and the topical steroid tapered. Long-term, the patient continues cyclosporine or lifitegrast twice daily.
Other Surgical Options
|
Systemic immunosuppression is important for the long-term success of the transplant. Using the Cincinnati Eye Institute protocol, clinicians start patients on medical treatment prior to surgery with oral prednisone 1mg/kg/day and tapered over one to three months, oral valganciclovir 225mg QD, trimethoprim/sulfamethoxazole (TMP/SMX) every MWF, oral tacrolimus 4mg BID and oral mycophenolate mofetil (MMF) 1g BID. Valganciclovir and TMP/SMX are stopped at 12 months, tacrolimus is tapered after six months and MMF after 12 months.
Although patients are free of medical treatment at three years, clinicians should monitor them closely for possible rejection.2
| 1. Cheung AY, Holland EJ. Keratolimbal allograft. Curr Opin Ophthalmol. 2017;28(4):377-81. 2. Holland EJ, Mogilishetty G, Skeens HM, et al. Systemic immunosuppression in ocular surface stem cell transplantation: results of a 10-year experience. Cornea. 2012;31(6):655-61. |

