 |
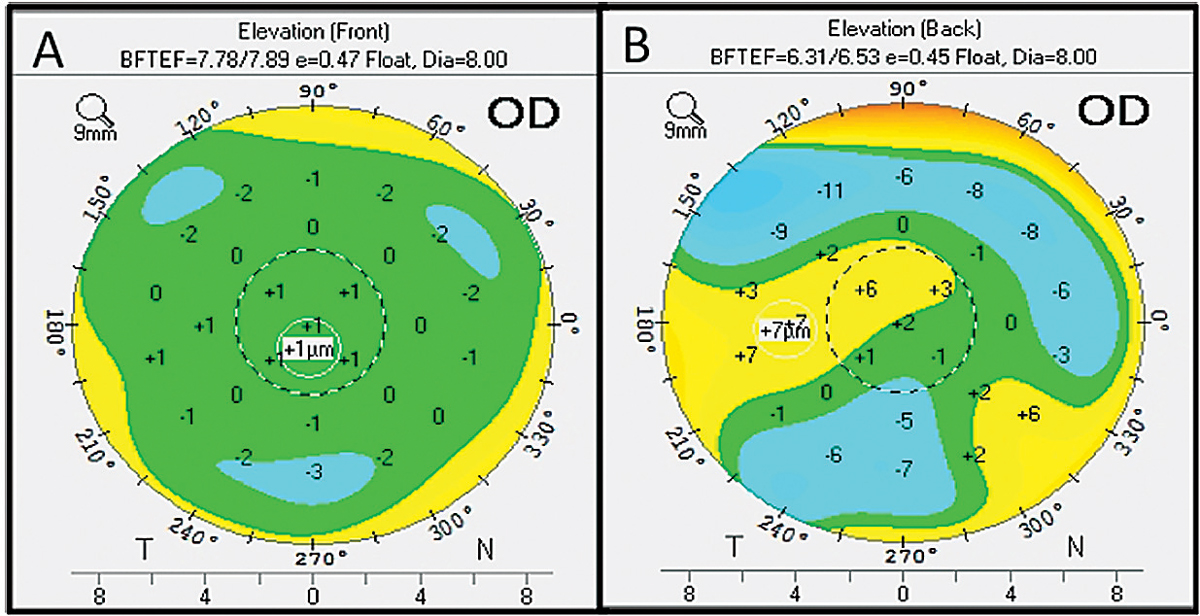
| Researchers noted that caution should be used when interpreting suspected elevation maps of potential refractive surgery candidates who don’t have any clinical or topographic aspects of keratoconus. Photo: Maria Walker, OD. Click image to enlarge. |
Screening refractive surgery candidates using topography is important to rule out keratoconus. However, not all elevation changes are due to that disease. Central astigmatism may also change the corneal elevation in otherwise normal cases, experts point out. To help rule out keratoconus in cases with beyond-normal elevation, researchers recently identified possible associations of corneal decentration indices and elevation values. They found that a larger angle kappa is associated with a more elevated cornea when using a best-fit sphere but not a best-fit toric ellipse.
The researchers assessed the right eyes of 173 refractive surgery candidates, including anterior and posterior corneal elevation maps, keratometric data, decentration indices and corneal astigmatism on Pentacam HR and angle kappa on Orbscan IIz. They compared their data with that of 148 age- and sex-matched controls with keratoconus grade one.
The researchers found that in normal refractive surgery candidates, mean angle kappa was 5.32°. They also reported that angle kappa had a positive correlation with anterior and posterior temporal elevation based on a best-fit sphere. Furthermore, anterior and posterior keratometric astigmatism was positively correlated with anterior/posterior nasal and temporal elevation and negatively correlated with superior and inferior elevation. The researchers pointed out that these associations went away when using a best-fit toric ellipse to calculate elevation data. They also noted that thinnest-point vertex decentration had a significant association with back-temporal elevation based on the best-fit toric ellipse in normal and keratoconus eyes.
The researchers concluded that caution should be used when interpreting suspected elevation maps of potential refractive surgery candidates who don’t have any clinical or topographic aspects of keratoconus. “In case of a suspected temporal elevation in the context of normal topographic features, we recommend using the best-fit toric ellipse instead of the best-fit sphere and assessing the relative pachymetry at the same time,” the researchers wrote in their paper. They say this approach should eliminate most cases of pseudo-elevation occurring due to astigmatism or large decentration. If elevation persists in a best-fit toric ellipse map, they recommend performing other tests such as biomechanical evaluation and epithelial/stromal OCT maps to exclude ectasia.
Salouti R, Nowroozzadeh MH, Azizi A, et al. Angle kappa and its effect on the corneal elevation maps in refractive surgery candidates. J Cataract Refract Surg. April 8, 2022. [Epub ahead of print]. |

