Elderly patients often present with a multitude of ocular and systemic conditions. When two eye diseases manifest in the same individual, is that a warning sign of greater concerns with their overall health? A team of researchers from Texas, Georgia and North Carolina investigated whether there is an increased propensity for systemic conditions in patients with both age-related macular degeneration (AMD) and glaucoma. They found that older age, inflammatory triggers and certain other mechanisms could tie the four conditions together. Results were recently published in Journal of Clinical Medicine.
 |
|
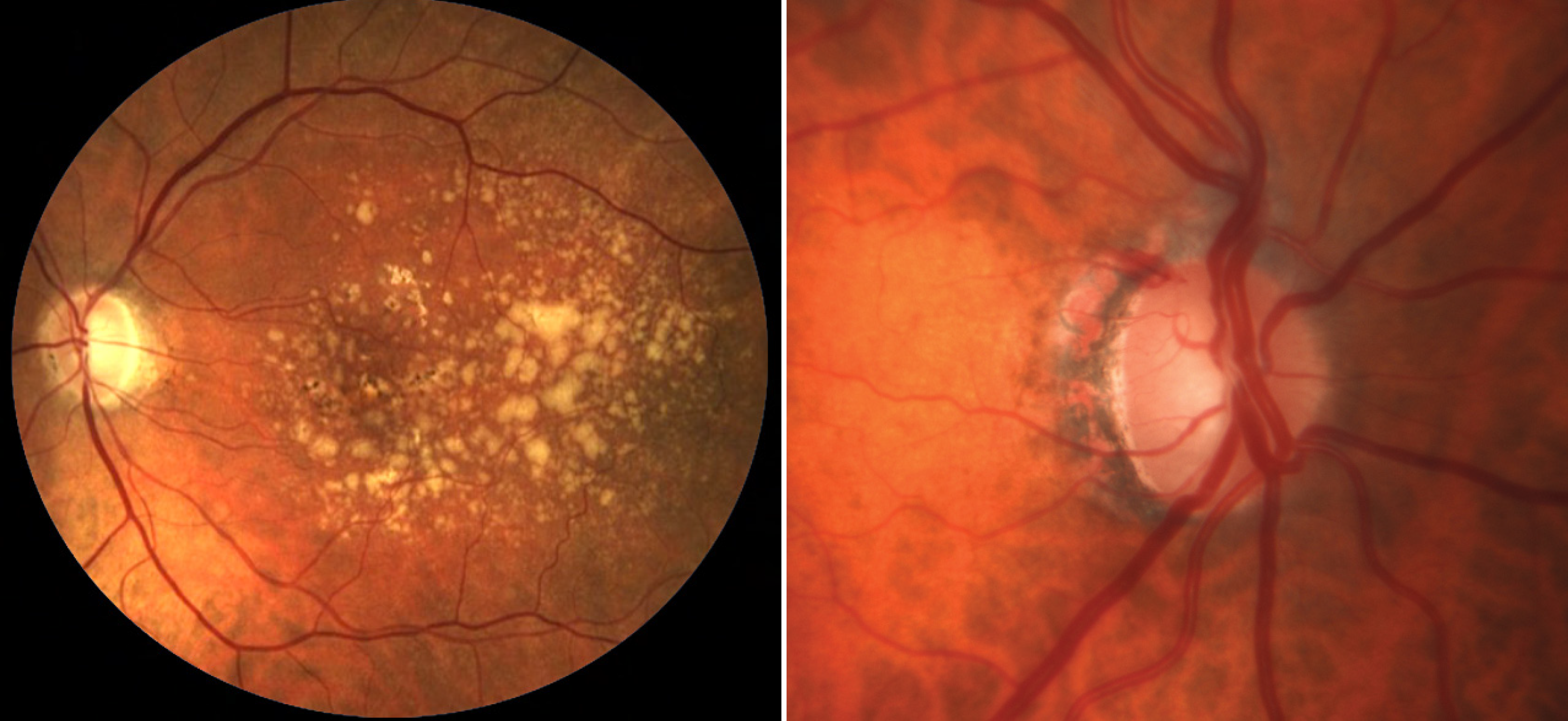
AMD and glaucoma individually indicate a high rate of systemic comorbidities, notably a higher prevalence of heart failure and dementia, than those with either disease alone. Photo: NEI; Michael Chaglasian, OD. Click image to enlarge. |
A large retrospective review was conducted using 14 years’ worth of data on patients seen at the University of North Carolina with the intent of identifying four groups: glaucoma only (5,243 patients), AMD only (6,726 patients), glaucoma plus AMD (402 patients) and cataracts only (25,450 patients). The systemic disease prevalence for each group was calculated and compared.
The study shows both AMD and glaucoma individually portend a higher rate of comorbidities than age-matched controls. Patients with these eye conditions demonstrate a uniquely higher prevalence of heart failure (HF) and dementia than those with either disease alone.
There are certain mechanisms that could connect heart failure, dementia, glaucoma and AMD. Heart failure can lead to decreased cerebrovascular blood flow, which has been associated with dementia and can also lead to decreased ocular perfusion, the authors noted in their paper. “The resultant ischemia in the eye, followed by reperfusion, can cause inflammation, which, either by itself or in addition to chronic ongoing inflammation, can lead to the development and progression of glaucoma and AMD,” they explained in the article.
Also pertinent is the role of inflammation. A low level of chronic systemic inflammation could be responsible for the maintenance and progression of heart failure, the authors suggested in the paper. “This could represent a state of increased pro-inflammatory cytokines and other inflammatory molecules circulating throughout the body, which could trigger dysregulation of mechanisms that are responsible for homeostasis of the immune system in the immune-privileged tissues, like the brain and retina.”
As patients with either AMD or glaucoma are typically older, they may simply be more likely to present with age-related cardiovascular risk factors. Increased age, the authors explained, can lead to the breakdown of normal functions meant to control inflammation, as well as an accumulation of oxidative stress and waste products, which can serve as triggers of inflammation.
“It is also possible that the presence of both AMD and glaucoma could indicate advanced disease or underlying pathophysiology that could potentially increase the risk of heart failure,” the authors wrote. “However, it is important to note that further pathophysiological investigations are required to fully understand the underlying mechanisms linking these conditions.”
The underlying association and pathologic mechanisms warrant further investigation to improve the overall health management and prognostication for these individuals. “Further studies may investigate the time course and progression of comorbidities, specifically HF and dementia, as well as of ocular conditions in patients with both glaucoma and AMD to further elucidate the specific pathologic mechanisms that may be driving these associations,” the authors concluded.
| Click here for journal source. |
Dimalanta L, Pithadia K, Shenkute NT, et al. Disease associations among patients afflicted with both glaucoma and age-related macular degeneration. J Clin Med. October 6, 2024. [Epub ahead of print.] |

