 |
The evaluation of the optic nerve is an essential part of any ocular health examination. The structure and integrity of the neuroretinal rim must be assessed, as well as the presence of adequate optic nerve perfusion. The presence or absence of distinct disc margins is noted as it is an essential clue in determining the etiology of disc swelling and/or suspected papilledema.
Frequently, the optometrist is faced with very subtle findings and is forced to decide whether these represent normal variations or something that warrants an emergent workup and referral. In such cases, the most helpful element of the examination is the presence or absence of a spontaneous venous pulse (SVP).
Clues in the Anatomy
To understand the clinical and physiologic importance of the SVP, it is important to recall the course of the optic nerve (ON). The ON runs from the retina towards the optic chiasm and is classified into four segments. The first is the intraocular segment, which measures only 1mm in length and is evident on routine funduscopic examinations at the level of the lamina cribrosa. The ON continues on as the intraorbital segment, which measures 20mm to 30mm and extends from the posterior globe to the orbital apex. Next is the intracanalicular segment (4mm to 9mm), which travels within the bony optic canal. Finally, the intracranial segment (10mm) extends from the optic canal to the optic chiasm.1
With the exception of the intraocular segment, the entirety of the ON is surrounded by the same meningeal layers as the brain—pia, arachnoid and dura. Furthermore, the subarachnoid space of the brain is contiguous with the subarachnoid space around the ON. Finally, it is important to remember that the central retinal vein and artery enter the intraorbital segment of the ON and continue towards the retina.
Because of these anatomic orientations, the ON and central retinal vein are exposed to, and influenced by, changes in intracranial cerebrospinal fluid (CSF) pressure.1
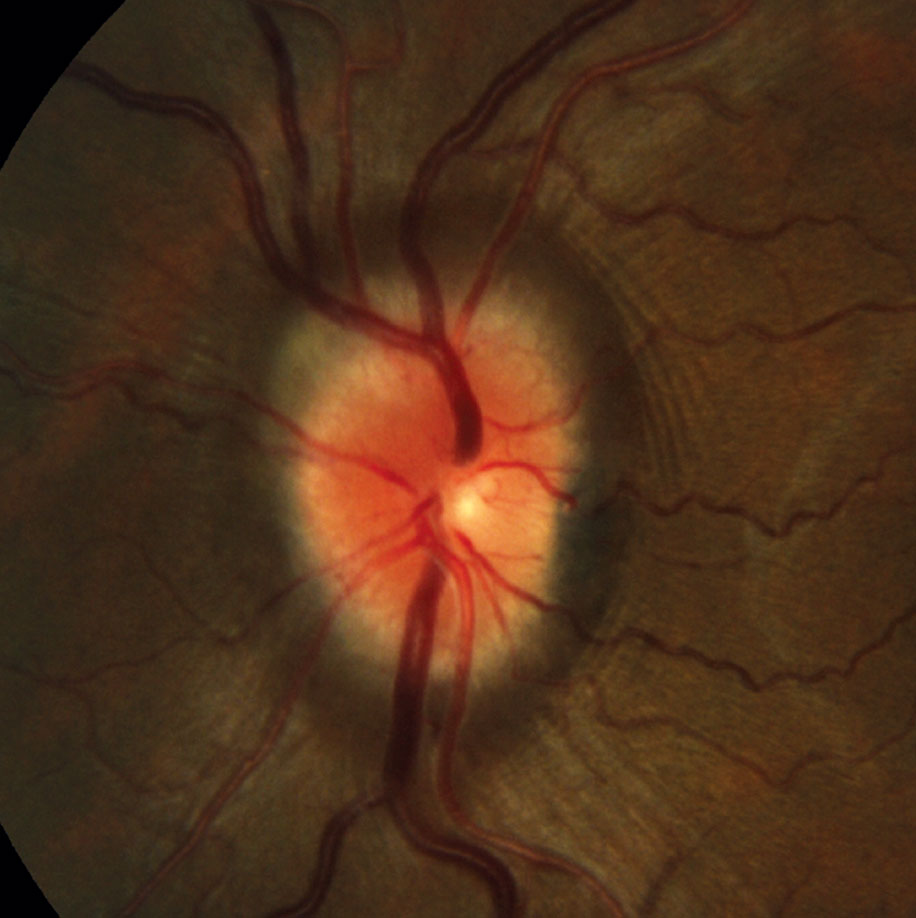 |
| Optic nerve swelling secondary to increased intracranial pressure with loss of SVP. |
What are the SVPs?
The phenomenon is defined as rhythmic pulsations occurring in the retinal vein(s) as they cross the optic disc.2 These pulsations are synchronized with the patient’s cardiac cycle, with the venous caliber steadily narrowing during systole and expanding with diastole.2-4
Because portions of the ON and central retinal vein are exposed to the subarachnoid space before traversing the lamina cribrosa, the pressure difference between the subarachnoid space and intraocular space gives rise to the SVP—in essence, the SVP is a physical manifestation of this pressure difference.2,3
Typically, the intraocular pressure is greater than the intracranial CSF pressure. However, when there is a rise in intracranial CSF pressure such that it equates to the intraocular pulse pressure, the SVP ceases to occur. This is because there is no longer a pressure gradient to produce the venous pulsation.2,4 This fact makes SVP an essential component in the evaluation of patients with suspected papilledema secondary to increased intracranial pressure—the documentation of an SVP will often rule out papilledema.
Since only 80% to 90% of normal, healthy eyes will exhibit SVP, its absence does not necessarily indicate an underlying pathological condition.2,5 An SVP may be absent in healthy patients due to certain optic disc configurations in which the pulsating retinal vein may be obscured by overlying retinal arteries or glial tissue as it enters the cup.4,6,7 Additional congenital variations, wherein the veins enter the optic disc peripherally instead of centrally in a shallow cup, may also obscure visibility.4
Even in patients with disc swelling that is not secondary to a rise in intracranial pressure, an SVP may be difficult to observe due to the local mechanical compression of the superficial veins.4 Because of these normal variants and special cases, the absence of an SVP in and of itself is not particularly helpful. Rather, the presence of an SVP or the loss of a previously documented SVP proves of the greatest clinical value in suspicious cases.
Clinical Relevance
SVPs are often crucial in the management of patients with subtle disc elevation in determining the need for an emergent workup to exclude a pathological manifestation of intracranial disease. As such, the eye care provider should be comfortable and skilled in looking for this subtle finding as part of a routine ocular health assessment, to either aid in ruling out disease processes or to document its presence or absence in healthy patients for future monitoring. The best way to check for an SVP is to use the direct ophthalmoscope, as it offers 15x magnification to best visualize the vessels through a dilated eye.2
A great deal of emphasis has been placed on the significance of SVPs in cases of suspected papilledema, but they also play a role in glaucoma, where SVPs are present in only 54% of patients.7,8 The subset of glaucoma patients most affected by a loss of SVP is normotensive, as they have been shown to have alterations in ocular and systemic perfusion and blood flow velocities.8 Preliminary studies suggest that the loss of an SVP may serve as a marker for glaucoma severity and progression.8
Although a subtle finding, a SVP can be a very telling sign and should be documented on routine ocular health assessments. The loss of a previously documented SVP may be a harbinger of underlying intracranial pathology in the setting of suspected papilledema. Furthermore, loss of a SVP may also indicate worsening glaucoma, possibly suggesting the need for more aggressive management.
1. Gala F. Magnetic resonance imaging of optic nerve. Indian J Radiol Imaging. 2015;25(4): 421–438. 2. Jacks AS, Miller NR. Spontaneous retinal venous pulsation: aetiology and significance. J Neurol Neurosurg Psychiatry. 2003;74:7-9. 3. Kim M, Ji Lee E, Seo Je, et al. Relationship of Spontaneous Retinal Vein Pulsation with Ocular Circulatory Cycle. PLoS ONE. 2014;9(5):1-5. 4. Lascaratos G, Ahmed S, Madill S. Spontaneous venous pulsation and its role in differentiating papilledema from pseudopapilledema. Neurology. 2010:e53-e54. 5. Morgan WH, et al. Retinal Vein Pulsation is in Phase with Intracranial Pressure and Not Intraocular Pressure. Physiology and Pharmacology. 2012;53:4676-4681. 6. Donelly SJ, Subramanian PS. Relationship of Intraocular Pulse Pressure and Spontaneous Venous Pulsations. 2009;147(1):51-55. 7. Morgan WH, et al. Intraocular Pressure Reduction is Associated with Reduced Venous Pulsation Pressure. PLOS ONE. 2016:1-9. 8. Pinto LA, et al. Lack of spontaneous venous pulsation: possible risk indicator in normal tension glaucoma? Acta Ophthalmologica. 2012;91:514-520. |

