 |
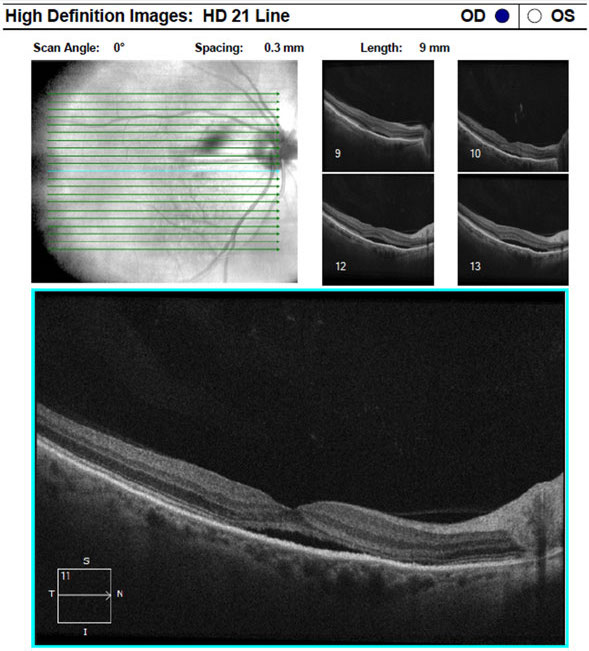
| It's not common for an nAMD patient on anti-VEGF therapy to develop SMH with vision loss, study shows. Photo: Amy Bade, OD. Click image to enlarge. |
A recent study gathered data from the Fight Retinal Blindness! registry on patients with nAMD treated with anti-VEGF. The objective was to report on the estimated incidence, cumulative rate, risk factors and outcomes of submacular hemorrhage (SMH) with loss of vision among the patient subset. While the data showed that SMH with loss of vision isn’t a common complication, it did reveal that the possibility exists at any time throughout treatment and that affected patients had only limited recovery of vision a year later.
There were 7,642 treatment-naïve eyes (6,435 patients) receiving anti-VEGF therapy included in the retrospective analysis. Patients received injections throughout a 10-year period, totaling 135,095 injections among the cohort. The researchers calculated the estimated incidence, cumulative rate and hazard ratios of SMH with loss of vision during treatment using various statistical models.
The rate of eyes that developed SMH with loss of vision was one per 1,283 injections (105 patients). The estimated incidence of SMH with loss of vision per year was 4.6 per 1,000 patients treated during the study period. Importantly, the researchers noted that the cumulative rate of SMH per patient was not significantly affected by the number of injections.
“The cumulative rate of SMH was 0.95% at 10 injections, 1.62% at 20 injections, 2.12% at 30 injections, 2.59% at 40 injections and 3.01% at 50 injections,” they wrote in their paper. “We did not find any clinically significant increase in the probability of SMH with each successive injection, even after more than 50 injections. Thus, each successive injection without a SMH did not seem to increase the risk of developing a SMH at the next injection.”
Patients with SMH had a mean visual acuity (VA) drop of approximately six lines at the time of diagnosis, which then improved moderately to a four-line loss after one year. The researchers wrote, “60% and 53% of SMH eyes had at least a two-line and three-line loss of vision from prior SMH at 12 months, respectively. A quarter of SMH eyes recovered their VA at 12 months, while half of the matched control eyes maintained their vision during the same period.” They noted that there was no difference in the average number of treatments and visits between cases and control subjects at 12 months.
The study also evaluated possible risk factors for the development of SMH during anti-VEGF treatment. In the cohort, men and eyes with disciform scar choroidal neovascularization type at baseline had a significantly higher rate of SMH development.
While visual outcomes after one year may be poor for patients who develop SMH from anti-VEGF injections, hemorrhage-induced vision loss is a very uncommon occurrence in this treatment population. Still, a low level of risk remains present throughout the treatment period.
Gabrielle PH, Maitrias S, Nguyen V, et al. Incidence, risk factors and outcomes of submacular hemorrhage with loss of vision in neovascular age-related macular degeneration in daily clinical practice: data from the FRB! registry. Acta Ophthalmol. March 23, 2022. [Epub ahead of print]. |

