 |
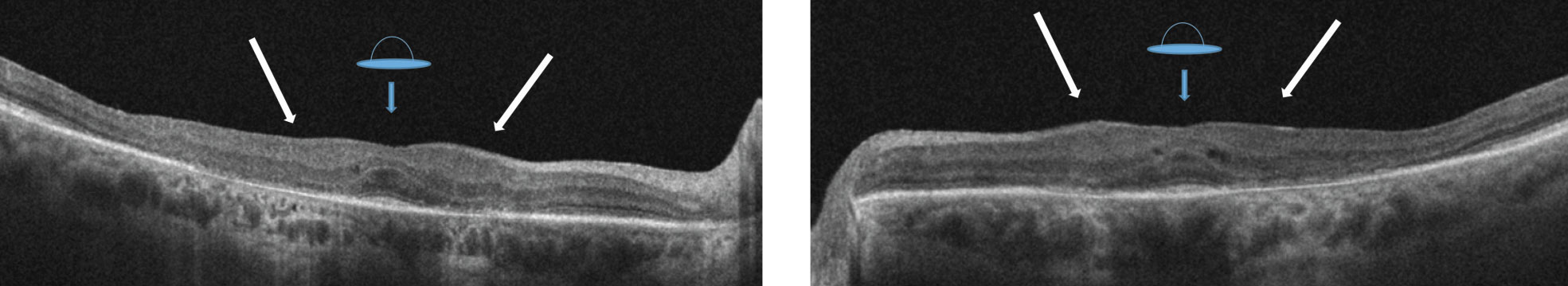
| Certain OCT biomarkers can indicate whether uveitis treatment was successful. Photo: Marlon Demeritt, OD. Click image to enlarge. |
Researchers recently identified two OCT biomarkers that may predict therapeutic response to treatment in eyes with macular edema. In a post-hoc analysis of two Phase III clinical trials, they analyzed BCVA and central subfield OCT features in noninfectious uveitis-related macular edema (NIU-ME). Though central subfield thickness has shown only limited correlation with BCVA, it’s still often used as an important secondary endpoint and component of retreatment criteria in ME clinical trials, the researchers pointed out in their paper.
“In clinical practice, physicians often base treatment decisions on both BCVA and OCT assessments,” they said, but lamented that “there’s limited literature on OCT anatomic and temporal biomarkers in ME due to NIU, the most common cause of vision loss in NIU.”
The researchers performed correlation and longitudinal treatment analyses on the Phase III data from the PEACHTREE and AZALEA trials in their clinical cohort study. A total of 198 patients had NIU, with 134 receiving suprachoroidally administered triamcinolone acetonide from Clearside Biomedical (CLS-TA) and 64 receiving sham. A total of 12.9% and 72% received rescue therapy, respectively.
The researchers observed BCVA progressively worsening at baseline with each ordinal drop in ellipsoid zone (EZ) integrity. They reported that eyes with a normal baseline EZ demonstrated a greater 24-week change in BCVA compared with eyes with some degree of baseline EZ disruption (11.9 vs. 9.4 letters, respectively). “In contrast, eyes without central subfield cystoid spaces and/or central subfield SRF at baseline showed less improvement at 24 weeks,” the researchers noted.
According to longitudinal modeling for CLS-TA-treated eyes, CST reached 90% of maximal improvement by week three, while a 90% maximal response in BCVA wasn’t reached until week nine. NIU-ME eyes that received CLS-TA and demonstrated a reduction of ≥50µm at four weeks had a greater 24-week improvement in BCVA compared with eyes without such an early response (14.6 vs. 6.5 letters, respectively).
“Integrity of EZ, also known as the photoreceptor IS/OS junction, reflects anatomic arrangement of photoreceptor outer segments and shows functional correlation in ME due to RVO, DME and NIU,” the researchers explained. “The current study demonstrated that mean baseline BCVA progressively worsened with deteriorating central subfield EZ grade in eyes with NIU” and correlated with the presence and location of central subfield cystoid spaces or subretinal fluid (SRF). “While mean BCVA progressively worsened with each central subfield EZ grade at baseline, these trends weren’t as strong of evidence for central subfield cystoid spaces or SRF gradation. However, eyes with baseline central subfield-involved cystoid spaces and/or SRF showed a significantly greater BCVA improvement at 24 weeks, compared with those without central subfield involvement. Consequently, central subfield cystoid spaces or SRF weren’t negatively prognostic features in these patients with NIU-ME.”
“It is intriguing that eyes with normal baseline central subfield EZ improved more than those with abnormal baseline central subfield EZ,” they continued, “while eyes without cystoid spaces and/or SRF in the central subfield at baseline improved less that those with central subfield involvement, possibly suggesting a floor effect for these latter two parameters.”
The researchers concluded, “Pre-treatment EZ integrity and the presence of subfield cystoid spaces of SRF each predict improved therapeutic response to treatment in eyes with NIU.” Additionally, they noted that anatomic improvement seemed to precede BCVA improvement by about one month.
Ciulla TA, Kapik B, Barakat MR, et al. OCT anatomic and temporal biomarkers in uveitic macular edema. Am J Ophthalmol. November 2, 2021. [Epub ahead of print]. |

