 |
|
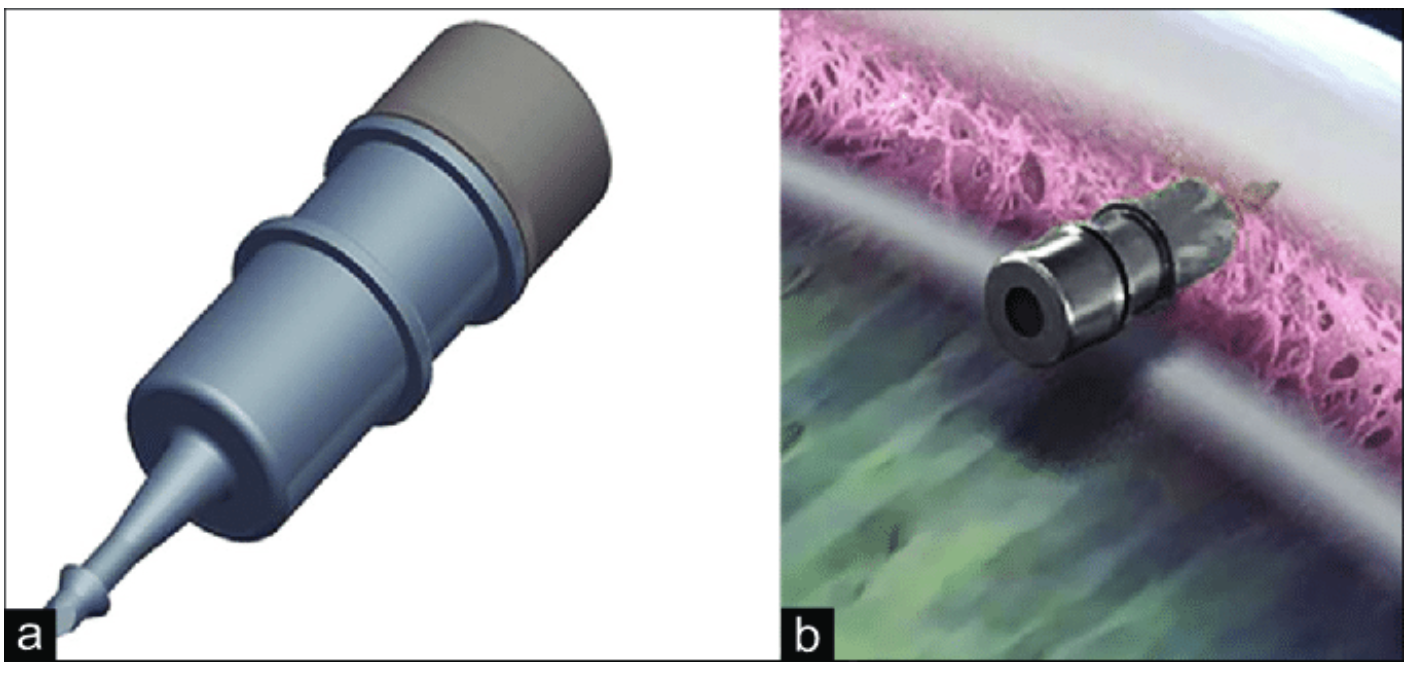
In a three-year Phase III trial, both fast- and slow-eluting implant models of iDose TR were well tolerated by patients and substantially reduced the burden of topical drops. Photo: Glaukos. Click image to enlarge. |
Poor adherence to medical therapy is associated with glaucomatous progression of visual field loss. Long-term IOP-lowering approaches can help to alleviate the patient burden that drops pose. Recently, researchers evaluated the safety and IOP-lowering efficacy of a new sustained release drug delivery system—the travoprost intraocular implant (iDose TR, Glaukos)—and found it to be noninferior to topical timolol.
In the pivotal Phase III trial, a fast-eluting (FE) implant and a slow-eluting (SE) implant were tested. Participants in the study included those with open-angle glaucoma or ocular hypertension using three or fewer IOP-lowering medications at the time of screening, with an unmedicated baseline mean diurnal IOP of 21 mmHg or greater and an unmedicated baseline IOP of 36mm Hg or less at each study timepoint (8am and 10am at day 10, week six and month three).
The researchers randomized study eyes to FE-implant (n=200), SE-implant (n=197) plus twice-daily placebo eye drops, or to sham plus timolol 0.5% (n=193). Over the six time points in the study, mean IOP reduction from baseline ranged from 6.6 to 8.4mm Hg for the FE-implant group, 6.6 to 8.5mm Hg for the SE-implant group, and 6.5 to 7.7mm Hg for the timolol group. The primary efficacy endpoint was met. The researchers also reported that adverse events occurred 21.5%, 27.2% and 10.8% of study subjects in the FE-implant, SE-implant and timolol groups, respectively. These included iritis, ocular hyperemia, reduced visual acuity and increased IOP. One study eye had endophthalmitis.
“The overall safety of the travoprost intraocular implants was favorable,” the researchers wrote in their Ophthalmology paper. “Although adverse events in the study eye were more common overall in the implant group than in the topical timolol group, the majority of these events were mild or moderate severity and did not compromise vision.” They added that although one study eye in the SE-implant group had endophthalmitis, endophthalmitis is a risk for all intraocular surgeries and injections. “It’s occurrence in this study highlights the importance of using proper aseptic technique upon administration and appropriate monitoring to ensure prompt treatment,” they wrote.
The researchers concluded that “the travoprost intraocular implant demonstrates robust IOP reduction that was non-inferior to timolol over a three-month primary efficacy evaluation period and provides a safe and effective alternative to topical IOP-lowering medication.”
Sarkisian SR, Ang RE, Lee AM, et al., on behalf of the GC-010 Travoprost Intraocular Implant Investigators. Phase 3 randomized clinical trial of the safety and efficacy of travoprost intraocular implant in patients with open-angle glaucoma or ocular hypertension. Ophthalmology 2024. [Epub ahead of print]. |

