 |
Q: The effect of Rhopressa (netarsudil, Aerie) on endothelial function is exciting, yet some patients have shown significant epithelial edema. What is the exact mechanism of this drop?
A: “The use of Rhopressa in the management of pathology of corneal endothelial cells (CECs) is a therapy in its infancy, but also one of the most exciting and active areas of publication in cornea literature,” according to Aaron Bronner, OD, of Pacific Cataract and Laser Institute in Kennewick, WA. Most of this research has been retrospective and case-based, but as of March, the first randomized clinical trial studied the use of Rhopressa in Fuchs’ dystrophy patients and reported an improvement in corneal thickness and visual acuity over three months.1
A medical approach to endothelial decompensation would be a revolutionary treatment, says Dr. Bronner, but notes the importance of having realistic expectations and recognizing potential complications, the most common of which is honeycomb epithelial edema.
|
|
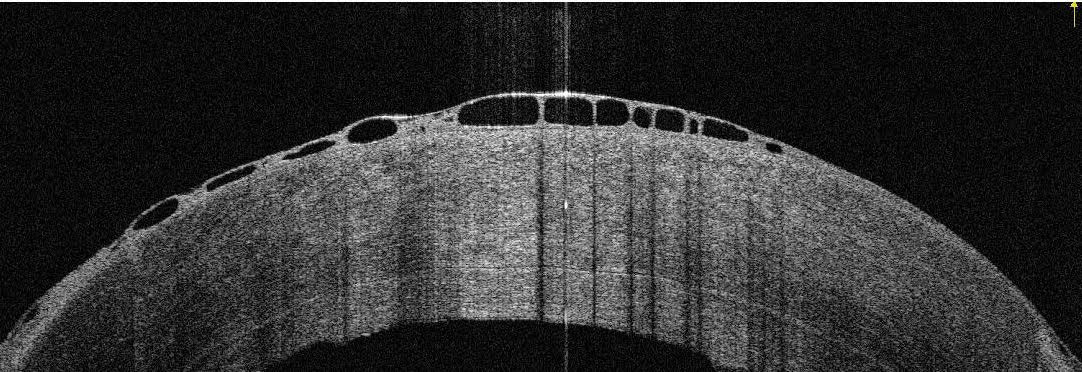
Honeycomb edema in a patient treated with Rhopressa who underwent a failed DSAEK. Photo: Aaron Bronner, OD. Click image to enlarge. |
The Nitty-Gritty
Honeycomb epithelial edema is concerning both in that it is extremely common in patients with corneal endothelial disease treated with netarsudil and that its presence seemingly flies in the face of the proposed benefit of the therapy, says Dr. Bronner, as these two outcomes are distinctly at odds.
The field is still in the early stages of research into this question, but based on available data and augmented by his own use of netarsudil in this population, Dr. Bronner believes that honeycomb epithelial edema counterintuitively does not cause an increase in corneal edema or have a negative influence on CECs. Instead, he thinks it’s probably associated with a change in the distribution of edema within corneas altered by ROCK inhibition. He notes that these eyes have not shown a consistent worsening of edema as measured by pachymetry.2 In fact, the eyes he has seen with honeycomb edema have surprisingly exhibited thinning. So, what is going on?
When establishing a cause of honeycomb edema, pinpoint where the problem is localized, who will develop it and the conditions that will help it clear. Although ROCK inhibitors are gaining attention for their role in endothelial healing, the endothelium isn’t the only cellular layer within the cornea that they impact. They also play a role in epithelial healing, cellular and intracellular junctions and maintenance of membrane permeability of epithelial cells.3,4
The at-risk patient profile is very specific. According to one review, honeycomb epithelial edema is nearly universal in patients treated with netarsudil who also have corneal edema or at least a significant risk factor for edema, but it doesn’t seem to occur in those treated with netarsudil who have a healthy endothelium.5 Therefore, both substantial CEC disease and netarsudil are necessary ingredients for the development of honeycomb edema. If either of these conditions change—the edema clears or the medication is discontinued—the honeycomb appearance will dissipate.2,5,6
Takeaways
The anterior localization of the problem, influence of ROCK inhibitors on cellular permeability of epithelial cells and requirement of pre-existing edema for the development of honeycomb edema make it very likely that this adverse effect reflects a change in the fluid balance in how epithelial cells respond to edema, rather than an impact on endothelial cells or a worsening of edema, Dr. Bronner notes.
Of course, this is all speculative. Time and research will shed light on the full picture, but for now, Dr. Bronner says he feels comfortable placing his patients with corneal edema on Rhopressa as an off-label way to attempt to improve corneal edema. In the event that honeycomb edema develops, he gives the medication up to a month longer. If it continues to persist, simply discontinuing the medication should result in its resolution with less of a risk for long-lasting harm.
Dr. Shovlin, a senior optometrist at Northeastern Eye Institute in Scranton, PA, is a fellow and past president of the American Academy of Optometry and a clinical editor of Review of Optometry and Review of Cornea & Contact Lenses. He consults for Kala, Aerie, AbbVie, Novartis, Hubble and Bausch + Lomb and is on the medical advisory panel for Lentechs.
1. Price MO and Price FW. Randomized, double-masked, pilot study of netarsudil 0.02% ophthalmic solution for treatment of corneal edema in Fuchs dystrophy. Am J Ophthalmol. 2021;227:100-5. 2. LoBue SA, Moustafa GA, Vu A, et al. Transient reticular cystic corneal epithelial edema with topical netarsudil: a case series and review. Cornea. December 22, 2020. [Epub ahead of print]. 3. Moshifar M, Parker L, Birdsong OC, et al. Use of rho kinase inhibitors in ophthalmology: a review of the literature. Med Hypothesis Discov Innov Ophthalmol. 2018;7(3):101-11. 4. Yin J, Yu FSX. Rho kinases regulate corneal epithelial wound healing. Am J Physiol Cell Physiol. 2008;295(2):C378-87. 5. Wisely CE, Liu KC, Gupta D, et al. Reticular bullous epithelial edema in corneas treated with netarsudil: a case series. Am J Ophthalmol. 2020;217:20-6. 6. Davies E. Case series: novel utilization of rho-kinase inhibitor for the treatment of corneal edema. Cornea. 2021;40(1):116-20. |

