 |
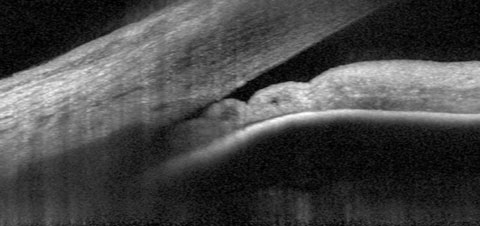
| One in four untreated PACS eyes in the ZAP trial data progressed to PAC within 14 years. Photo: James L. Fanelli, OD. Click image to enlarge. |
Evaluating the risk of angle closure in primary angle closure suspect (PACS) eyes is crucial for optometrists to determine appropriate management and assess the need for early laser peripheral iridotomy (LPI). Factors that increase this risk are underreported, which recently provoked researchers to analyze data from the Zhongshan Angle Closure Prevention (ZAP) trial to develop prediction models for the 14-year risk of progression from PACS to primary angle closure (PAC). They identified three variables to predict progression: IOP, central anterior chamber depth (ACD) and limbal ACD.
The cohort study involved 377 untreated PACS eyes from 377 patients (84% female; mean age: 58 years). Baseline examinations included tonometry, ultrasound A-scan biometry and anterior-segment OCT. Primary angle closure was defined as peripheral anterior synechiae in one or more clock hours, IOP above 24mm Hg or acute angle closure.
By the 14-year follow-up, 93 eyes (25%) had progressed from PACS to angle closure. The multivariate analysis revealed the following baseline predictors of progression:
- higher IOP (odds ratio, OR: 1.14 per 1mm Hg increase);
- shallower central ACD (OR: 0.81 per 0.1mm increase); and
- shallower limbal ACD (OR: 0.96 per 0.01 increase in peripheral corneal thickness).
As for AS-OCT measurements, the following baseline factors were identified as predictors for the 14-year risk of progression: smaller light-room trabecular-iris space area (TISA) at 50μm from the scleral spur (OR: 0.86 per 0.01-mm2 increase), smaller light-room angle recess area (ARA) at 750μm from the scleral spur (OR: 0.93 per 0.01mm2 increase) and smaller dark-room TISA at 500μm (OR: 0.89 per 0.01mm2 increase).
“Based on IOP and central and limbal ACDs, logistic regression models showed moderate performance (area under the curve: 0.69) in predicting the long-term risk of progression in untreated PACS eyes,” the researchers reported in their study, published last week in JAMA Ophthalmology.1 In addition, the inclusion of AS-OCT metrics didn’t appear to improve predictions, leading the authors to suggest that the parameters of IOP, central ACD and limbal ACD may suffice to identify eyes at high risk of angle closure. “With limbal ACD replaced by AS-OCT parameters, alternative models had comparable performance in predicting progression from PACS to PAC within 14 years,” they wrote.
When determining if a PACS patient would benefit from prophylactic LPI—which, when performed early, has been associated with improvement in the clinical course of angle closure—the author of an invited commentary, also published in JAMA Ophthalmology, agrees that current evidence supports that this decision can be made based on IOP, central ACD and limbal ACD; however, these aren’t the only factors that need to be considered, he clarified.2
“In addition to the comprehensive ocular examination (including dynamic gonioscopy), patient factors such as age, sex, race, ethnicity, and refractive status should be considered since risk factors for the development of PAC glaucoma include older age, Asian race, female sex, hyperopia and positive family history,” the commentary author wrote.
The cohort study found the 15-minute dark room prone provocative test to help derive additional IOP data from patients with asymptomatic PACS, another point that the commentary agreed with. “The test has been reported to be a safe and effective method in eliciting IOP increases of at least 8mm Hg to diagnose intermittent angle closure associated with pupillary block,” its author noted.2 However, he pointed out that it’s important for clinicians “to recognize that prophylactic LPI will only eliminate the pupillary block component in eyes with PACS, and that the effectiveness of LPI in slowing the progression of visual field loss in these eyes is uncertain. Furthermore,” he continued, “laser iridoplasty is more effective than LPI for mechanisms of angle closure other than pupillary block, such as plateau iris syndrome, a common cause of PACS in younger patients.”
For patients who may not benefit from laser therapy, “such as younger patients with plateau iris syndrome with normal IOP levels, no evidence of PACS and no acute angle closure symptoms or signs,” the author of the commentary suggests that observation may be a reasonable alternative.
In summary, the study authors concluded in this paper that “higher IOP, shallower central and limbal ACDs, and smaller TISA at 500μm and light-room ARA at 750μm may serve as baseline predictors for progression to PAC in PACS eyes. Evaluating these factors can aid in customizing PACS management.”1
1. Yuan Y, Xiong R, Wang W, et al. Long-term risk and prediction of progression in primary angle closure suspect. JAMA Ophthalmol. January 18, 2024. [Epub ahead of print]. 2. Tsai JC. Invited Commentary: Longitudinal management of primary angle closure suspect. JAMA Ophthalmol. January 18, 2024. [Epub ahead of print]. |

