 |
A 62-year-old black male presented for a comprehensive eye examination with complaint of blurry vision at distance for a year. Medical history included Type 2 diabetes mellitus for five years, hypertension and hypercholesterolemia, for which he was on oral medications. His reported glycosylated hemoglobin (HbA1c) was 8.0.
Ocular examination revealed best-corrected visual acuities of 20/30 OD and 20/25 OS. Pupils, ocular motilities and confrontation visual field were unremarkable. Mild nuclear sclerotic cataracts were observed on slit-lamp evaluation in both eyes. Of note was an area of vascular abnormality on his right optic disc. Mild retinal hemorrhages, arteriovenous nicking and macular changes were noted in his right eye (Figures 1 and 3). Dilated examination of his left eye revealed a healthy optic disc and arterio-venous nicking (Figure 2). SD-OCT was performed as well (Figure 4).
 | 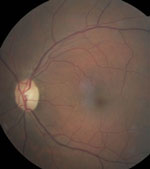 | |
| Figs. 1 and 2. Above, can you diagnose this 62-year-old black male who presented with blurry vision at distance using these fundus photos of the right and left eyes? Fig. 3. At right, look carefully at the optic nerve of the right eye. | 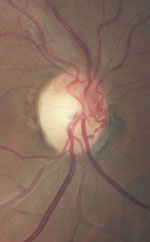 |
Take the Quiz
1. What do the changes seen on the optic nerve photo represent?
a. Optic disc hemorrhage.
b. Neovascularization.
c. Collateral retinochoroidal vessels.
d. Optic disc capillary hemangioma.
2. What does the SD-OCT finding of the right eye reveal?
a. Clinically significant macular edema (CSME).
b. Vitreomacular traction (VMT).
c. Non-center involved diabetic macular edma.
d. Epiretinal membrane.
3. Based on the clinical findings, what is the correct diagnosis?
a. Resolving central retinal vein occlusion (CRVO).
b. Asymmetric diabetic retinopathy.
c. Ocular ischemic syndrome.
d. VMT.
4. What is the likely etiology?
a. Carotid artery stenosis.
b. Hypertension.
c. Sickle cell disease.
d. Idiopathic.
5. How should the ocular findings be managed?
a. Intravitreal anti-VEGF injection.
b. Topical steroid/NSAID.
c. Pars plana vitrectomy.
d. Intravitreal ocriplasmin injection.
For answers, see below.
Discussion
The changes involving the optic nerve of the right eye represent neovascularization. On close inspection, fine wispy vessels are visible from 1:00 to 3:00 on the disc. xIn addition, there were scattered blot hemorrhages, and the SD-OCT revealed cystoid macular edema. This appears to be early proliferative diabetic retinopathy (PDR). We expected to see similar changes in the left eye, but upon close inspection, the left eye was essentially normal with the exception of mild A/V nicking. Our patient appears to have asymmetric diabetic retinopathy with PDR and CSME in the right eye and no diabetic retinopathy in the left eye. So, what is going on?
Diagnoses
Asymmetric DR is defined as proliferative diabetic retinopathy in one eye and nonproliferative diabetic retinopathy or no retinopathy in the fellow eye.1,2 It is a rare disease, occurring in 5% to 10% of patients with diabetes.3 Several factors have been linked to asymmetric DR, including vitreous loss from cataract surgery, trauma, uveitis, optic atrophy, branch retinal vein occlusion, PVD, chorioretinal atrophy, amblyopia and high myopia.1-3 A predominant factor inducing asymmetric DR is carotid artery disease, which has been found to occur in four of 20 patients with asymmetric PDR.1
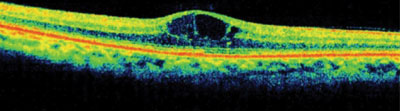 | |
| Fig. 4. SD-OCT images of the right and left macula—what does the OCT reveal? |
The disease presents with no mild retinopathy on the same “ipsilateral” side as the more stenotic carotid artery, which is thought to be “protective” against the development of PDR. Although not clearly understood, researchers speculate that the protective effect results from a reduction of retinal arterial perfusion pressure.4 Asymmetric DR should also raise suspicion of venous stasis retinopathy or ocular ischemic syndrome (OIS), which is characterized by uveitis, iris neovascularization and mid-peripheral retinal hemorrhages and microaneurysms. OIS develops on the ipsilateral side as the severe stenosis and is associated with a five-year mortality of 40%.5
Additional Testing
Given these concerns, we listened for a bruit by performing carotid artery auscultation on our patient and were surprised to hear one on the left side. We then referred our patient for carotid ultrasound and Doppler testing, which revealed 50% stenosis of the right carotid and 65% stenosis of the left carotid. Due to lack of symptoms, such as transient ischemic attack (TIAs) or dizziness, carotid artery endarterectomy was deferred and the patient was placed on aspirin (Ecotrin) 81mg daily therapy. His retinopathy was treated with anti-VEGF therapy and the cystoid macular edema resolved.
This case underscores the importance of recognizing this condition and its association with severe carotid artery disease. Prompt medical testing and intervention is essential with this condition to prevent not only vision loss, but also life-threatening complications or early death.
This case was written and provided by Sherrol Reynolds, OD, associate professor of optometry, Nova Southeastern University College of Optometry.
1. Duker J, Brown G, Bosley T, et al. Asymmetric proliferative diabetic retinopathy and carotid artery disease. Ophthalmology. 1990;97:869–74.2. Valone J, McMeel J, Franks E. Unilateral proliferative diabetic retinopathy. Initial findings. Arch Ophthalmol. 1981;99:1357–61.
3. Valone J, McMeel J, Franks E. Unilateral proliferative diabetic retinopathy. II. Clinical course. Arch Ophthalmol. 1981;99:1362-6.
4. Brown G, Magargal L, Simeone F, et al. Arterial obstruction and ocular neovascularization. Ophthalmology. 1982;89:139-44.
5. Sivalingam A, Brown G, Magargal L, Menduke H. The ocular ischemic syndrome. II. Mortality and systemic morbidity. International Ophthalmology. 1989 May;13(3):15-20.
Retina Quiz Answers:
1) b; 2) a; 3) b; 4) a; 5) a.

