 |
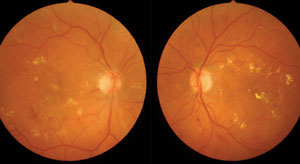
The FAc implant for DME appears to be effective and safe in long-term treatment. Photo: Paul Chous, OD. Click image to enlarge. |
Diabetic macular edema (DME) is usually treated with anti-VEGF agents, according to the standard of care. However, this therapy addresses only part of the DME pathogenesis (DME is also thought to be associated with chronic, low-grade inflammation that precedes and underlies vascular changes) and isn’t always the best option for patients due to both the treatment and cost burdens and the fact that not all patients respond well to anti-VEGF.
Another treatment route for patients lies with corticosteroids, such as a non-biodegradable 0.19mg fluocinolone acetonide (FAc) intravitreal implant (Iluvien, Alimera Sciences). Iluvien was FDA-approved in 2014 for treating DME in “patients who have been previously treated with a course of corticosteroids and did not have a clinically significant rise in intraocular pressure (IOP).”
FAc is a corticosteroid with low water solubility, allowing it to preferentially enter ocular tissue upon injection. The implant is formulated with submicrogram doses of corticosteroid that are released into the vitreous for up to 36 months. Such low doses are thought to reduce the incidence of steroid-related adverse events.
So far, Iluvien has demonstrated good clinical safety. The Phase III FAME study found that at 36 months, patients with DME who received the FAc implant had significantly higher rates of BCVA improvement of ≥15 letters and a lower rate of off-label DME rescue treatment compared with sham treatment.
Now, the three-year safety results of a Phase IV trial, PALADIN (NCT02424019), add more evidence that this sustained-release implant improves visual outcomes and reduces the treatment burden while maintaining a good safety profile. In the study, patients received a 0.19mg FAc intravitreal implant at baseline and were observed for up to 36 months. Primary safety outcomes included IOP changes and interventions to manage IOP elevations. Secondary outcomes included BCVA, central subfield thickness (CST) and adjunctive DME treatment frequency.
By the end of the study period, patients’ functional and structural outcomes improved, with a mean BCVA increase of 3.6 letters and a mean CST decrease of 60.7µm compared with baseline. In fact, seven days post-implantation, the researchers observed statistically significant visual acuity increases and CST decreases, both of which remained significant for the rest of the study duration.
The researchers also reported a treatment burden decrease of 67.6% with the sustained-release implant. In the three years prior to the study, participants had an overall median treatment frequency of 3.4 treatments per year, but during the study period this decreased to just one treatment per year. Additionally, among the 36-month “completer group” (n=94), 25.5% of eyes remained treatment-free through 36 months. A total of 108 enrolled eyes (32.8%) didn’t complete all 36 months because the study protocol called for the discontinuation of fellow eyes once the study eye completed 36 months. Seventy-three eyes (36%) discontinued the study for other reasons, including loss to follow-up. The researchers said this 12% per year discontinuation rate is consistent with other three-year studies.
Throughout the study, mean IOP remained stable. The researchers observed IOP increases >30mm Hg in 10.9% of eyes. They reported that IOP-related procedures were few, with a surgical rate of 2.97% with 1.5% attributable to steroids (as opposed to surgeries due primarily to neovascular glaucoma). Standard treatments were used to manage the 202 eyes with IOP increases. The researchers also noted that IOP response below 25mm Hg after steroids predicted that 96.9% of eyes would have a similar outcome with the implant at the final follow-up visit.
In one of the interim PALADIN analyses that included observational data preceding the FAc implant, the researchers observed visual losses. “During the [36 months] before FAc administration,” they wrote in their study, “patients with a baseline BCVA of 20/40 or better lost an average of eight letters, and those with a BCVA of worse than 20/40 at baseline lost an average of 10 letters despite the majority of patients having received prior DME Treatment with intermittent therapies, including anti-VEGF, steroids and laser therapies. In the 36 months of the PALADIN study, eyes didn’t lose letters but in fact gained letters.”
The researchers wrote that evolving research suggests DME is multifactorial and involves “numerous inflammatory cytokines and growth factors, one of which is VEGF.” “However, despite monthly anti-VEGF therapy, the DRCR.net Protocol T demonstrated that up to 65.6% of eyes with DME that were treated still had persistent DME at 24 weeks. This indicates that in many cases, anti-VEGF monotherapy alone isn’t sufficient to resolve signs of DME and suggests factors other than VEGF are at play in disease pathogenesis.”
Combination anti-VEGF and corticosteroid therapy could offer some help. Corticosteroids inhibit Ang2 as well as VEGF. FAc in particular, as a glucocorticoid receptor agonist, can suppress the production of inflammatory cytokines and growth factors via the FAc-receptor complex, which regulates the activities of transcription factors such as NFkB. The researchers noted the 0.19mg FAc implant is a “durable therapy option…with a comparable benefit-to-risk ratio to other FDA-approved corticosteroids for the treatment of DME, such as the dexamethasone implant.”
Despite the good safety outcomes of the phase 4 study, the researchers said that steroid-related events still warrant attention. In the PALADIN study, 18 of the 29 phakic eyes required cataract extraction. A previous cross-study comparison between the FAME and DRCR Protocol I noted that patients receiving FAc had higher incidences of cataract formation compared with those receiving ranibizumab. At three years in the FAME trial, cataract development requiring extraction occurred in 80% of phakic eyes compared with 14% at two years in the DRCR Protocol I.
“One important aspect of this study was the ability to predict IOP responses following the 0.19mg FAc implant in comparison to the IOP response from a prior steroid,” the researchers wrote in their paper. “The positive predictive value describes the probability of an IOP response post-FAc implant remaining ≤25mm Hg if the prior corticosteroid IOP response was also ≤25mm Hg. In this study an IOP response ≤25mm Hg to prior steroid is highly predictive of a similar IOP response at the end of the study post-FAc [96.9% for all 202 eyes and 95.6% for the 94 36-month completers]. Though post-FAc IOP elevations can occur, they are treatable, and the difference in IOP from baseline becomes insignificant by the end of the study. Again, this predictability aligns with both the interim PALADIN results (97.8%) and the USER study (98%).”
The researchers concluded that the benefit-risk profile of the implant is positive for long-term use in real-world populations with DME. They noted the reduced treatment burden, compared with other approved DME treatments, is a strong benefit, as are the improved visual outcomes, reduced macular edema and low incidence of IOP-related safety concerns.
Singer MA, Sheth V, Mansour SE, et al. Three-year safety and efficacy of the 0.19-mg fluocinolone acetonide intravitreal implant for diabetic macular edema: the PALADIN study. Ophthalmology. January 18, 2022. [Epub ahead of print]. |

