 |
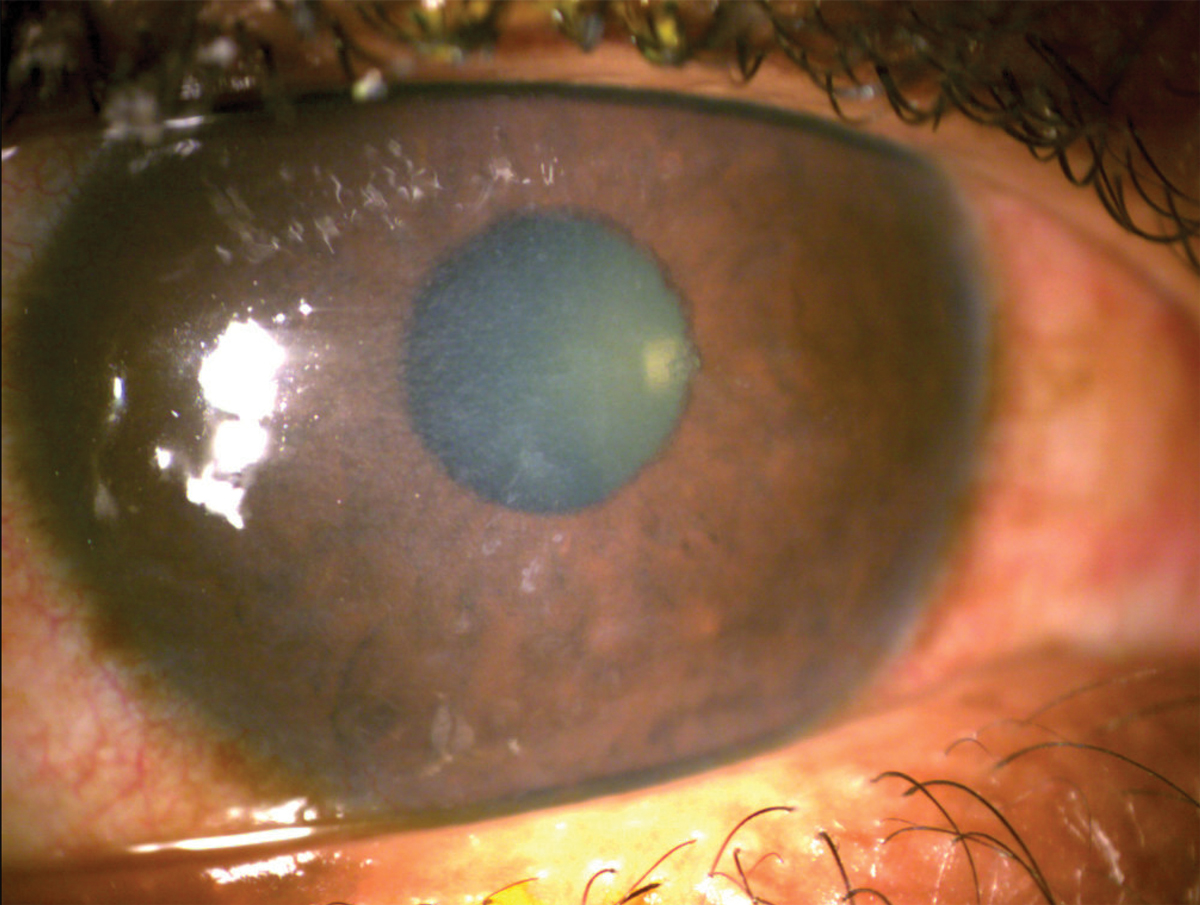
A 44-year-old man presented with a red, painful right eye with reduced vision, which began immediately upon waking that morning. He reported significant headache on the right side with radiating pain through his neck and back as a result of the ocular discomfort. He had established history of lattice corneal dystrophy and reported a similar experience in his left eye two years prior. Pinhole visual acuity was 20/200 OD and 20/60 OS. He manifested a large central corneal erosion with stromal haze, without corneal infiltrate. The fellow eye had refractile, branching stromal lesions with associated haze and subepithelial irregularity.
Recurrent corneal erosion is a known complication of lattice corneal dystrophy, a bilateral, progressive group of genetically inherited conditions.1 Genetic mutations in the transforming growth factor beta-induced (TGFBI) gene result in a spectrum of corneal dystrophies that can be clinically differentiated, including lattice corneal dystrophy, which is characterized by its branching filamentous opacities of amyloid fibers in the stroma.1 Specific genetic mutations may be determined through commercially available gene panels to inform specific lattice degeneration variants.1
Management of recurrent corneal erosion is threefold and involves treatment aimed to reduce risk of infection, promote corneal healing and manage associated discomfort. Prophylaxis of infection is addressed with a topical antibiotic. Oral over-the-counter acetaminophen, NSAID or both in combination, with consideration of a bandage contact lens and cycloplegia, are typically sufficient for pain management.
Treatment adjuncts to improve corneal healing and to reduce fibrosis including doxycycline or vitamin C are based on understanding of the complexities of the corneal wound healing response. Topical ophthalmic losartan has also been demonstrated to improve stromal haze and fibrosis in animal models and in isolated case reports which may represent an additional treatment consideration.
 |
|
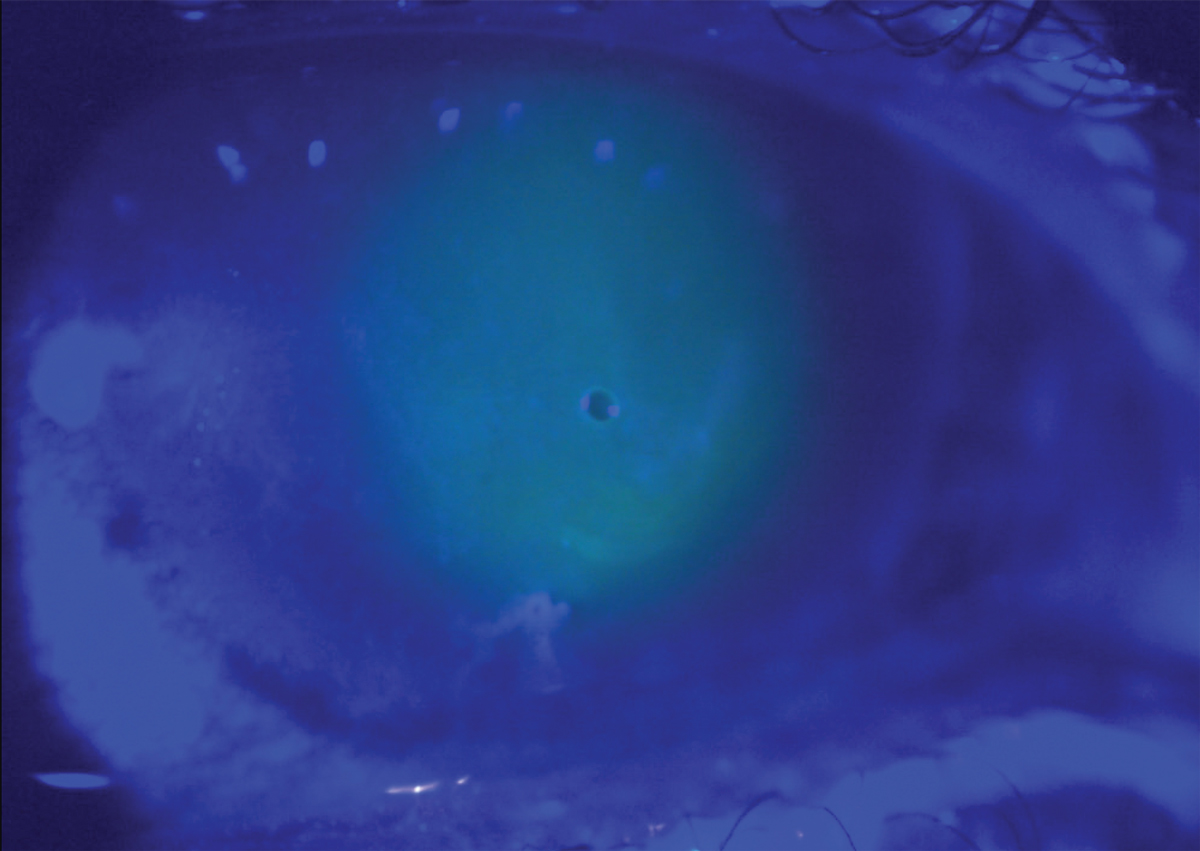
Large corneal erosion in a patient with lattice corneal dystrophy with bandage contact lens in place. Click image to enlarge. |
Matrix Metalloproteinases (MMPs)
These proteolytic enzymes are involved in processes ranging from biological signaling in cell adhesion, proliferation and migration, to degradation of extracellular matrix (ECM) components including collagen, gelatin and elastin.2,3 The physiologic inhibitors and mediators of MMPs are tissue-specific inhibitors. In the cornea, these are present in endothelial, epithelial and stromal cells and a careful physiologic balance between them and MMPs is required for extracellular matrix homeostasis, where imbalance and upregulation of MMPs can lead to tissue degradation.2
Of the 28 MMPs identified, MMP-9 is often discussed in the context of corneal disease due to its role in promotion of corneal inflammation.2 MMP-9 upregulation occurs early in corneal wound healing, with overexpression leading to chronic epithelial defect and inhibition resulting in improved epithelial basement membrane regeneration.2-4 An intact epithelial basement membrane is a requirement to prevent recurrent epithelial defects, corneal myofibroblast recruitment, and scarring.2-4 As MMP-9 is upregulated very early in the corneal healing process, inhibition through the use of systemic tetracyclines is supported in acute corneal erosion; however, as there has not been demonstrated elevation of MMP-9 levels in corneal epithelial cells once an erosion is healed, the long-term use for reduction of recurrence of RCE has been challenged.2,3
 |
|
Irregular epithelium following reepithelialization post-corneal erosion in lattice corneal dystrophy. Click image to enlarge. |
Vitamin C
This has also been proposed to have a therapeutic impact on corneal wound healing. Experimental data suggest vitamin C promotes the expression of markers in corneal epithelial stem cells, enhances collagen synthesis as well as ECM production and, as a strong antioxidant, reduces reactive oxygen species within the corneal epithelium.5
A retrospective evaluation of individuals with infectious keratitis determined that individuals who received oral (3g/day) or intravenous (20g/day) vitamin C had reduced size of corneal opacity in comparison with those who received standard treatment, with proposed efficacy of vitamin C to be greater in more highly inflamed eyes (younger individuals and those with hypopyon present).5,6 Of note, doses of vitamin C greater than 1g per day can increase likelihood of kidney stones and can falsely elevate blood glucose measurement.7,8
Topical Losartan
This medication has also been explored for its role in reduction of corneal scarring. Losartan has been proposed to result in apoptosis of myofibroblasts in the corneal stroma, which then allows for corneal fibroblasts to reorganize the extracellular matrix and for regeneration of the epithelial basement membrane.9,10 With impressive animal model data following alkali burn and isolated clinical case reports, topical losartan has emerged as a therapy of interest for corneal scarring.9,10
The theoretical potential in reduction of TGFBI-protein deposition in lattice corneal dystrophy exists due to losartan’s downstream effect of inhibiting TGF-ß signaling; however, its role in prevention of corneal fibrosis or role in recurrent corneal erosion, specifically in the context of corneal dystrophies, has not been supported.9
Case Management
In the patient case presented, a bandage contact lens (senofilcon A), was inserted and he was prescribed besifloxacin 0.6% TID for prophylaxis of infection. He was recommended to begin oral acetaminophen 500mg (maximum 3000mg daily) for pain and was prescribed doxycycline monohydrate 100mg BID. He was advised on the potential for gastrointestinal upset and phototoxicity and was recommended to take doxycycline with a full glass of water and with meals.
To reduce the likelihood of esophagitis, he was also advised to not to lay down for at least 30 minutes after taking doxycycline. Of note, we did not prescribe a topical NSAID due to the drug’s potential to delay healing. By day five, he was completely reepithelialized and had self-discontinued acetaminophen. On day seven, visual acuity had returned to baseline of 20/50 OD, the bandage contact lens was removed, besifloxacin was discontinued, and doxycycline was reduced to 100mg daily. He was offered genetic testing to inform family members of risk factors and referral for consideration of phototherapeutic keratectomy, both of which he has declined at this juncture.
Dr. Steen is an associate professor at Nova Southeastern University College of Optometry where she serves as director of the Glaucoma Service, coordinator of the Primary Care with Emphasis in Ocular Disease Residency and teaches courses in glaucoma and ocular pharmacology. Her financial disclosures include Bausch & Lomb, Santen, Ocuphire and Carl Zeiss Meditec.
1. Kheir V, Cortés-González V, Zenteno JC, et al. Mutation update: TGFBI pathogenic and likely pathogenic variants in corneal dystrophies. Hum Mutat. 2019;40(6):675-93. 2. Jadczyk-Sorek K, Garczorz W, Bubała-Stachowicz B, et al. Matrix metalloproteinases and the pathogenesis of recurrent corneal erosions and epithelial basement membrane dystrophy. Biology (Basel). 2023;12(9):1263. 3. Fini ME, Parks WC, Rinehart WB, et al. Role of matrix metalloproteinases in failure to re-epithelialize after corneal injury. Am J Pathol. 1996;149(4):1287-302. 4. Dursun D, Kim MC, Solomon A, et al. Treatment of recalcitrant recurrent corneal erosions with inhibitors of matrix met-alloproteinase-9, doxycycline and corticosteroids. Am. J. Ophthalmol. 2001;132(1):8-13. 5. Chen J, Lan J, Liu D, et al. Ascorbic acid promotes the stemness of corneal epithelial stem/progenitor cells and accelerates epithelial wound healing in the cornea. Stem Cells Transl Med. 2017;6(5):1356-65. 6. Cho YW, Yoo WS, Kim SJ, et al. Efficacy of systemic vitamin C supplementation in reducing corneal opacity resulting from infectious keratitis. Medicine (Baltimore). 2014;93(23):e125. 7. Yoo EH, Lee SY. Glucose biosensors: an overview of use in clinical practice. Sensors (Basel). 2010;10(5):4558-76. 8. Doseděl M, Jirkovský E, Macáková K, et al.; On Behalf Of The Oemonom. Vitamin c-sources, physiological role, kinetics, deficiency, use, toxicity and determination. Nutrients. 2021;13(2):615. 9. Wilson SE. Topical losartan: practical guidance for clinical trials in the prevention and treatment of corneal scarring fibrosis and other eye diseases and disorders. J Ocul Pharmacol Ther. 2023;39(3):191-206. 10. Martinez VV, Dutra BAL, Santhiago MR, Wilson SE. Effect of topical losartan in the treatment of established corneal fibrosis in rabbits. Transl Vis Sci Technol. 2024;13(8):22. |

