 |
A 42-year-old Dominican male presented with eight days of vision loss and photophobia of the left eye. He denied any associated flashes, floaters, recent trauma or similar symptoms in the right eye, which was asymptomatic. His past medical and ocular histories were unremarkable, and he was not taking any prescription or over-the-counter medications. He had no known environmental or drug allergies. An extended review of systems revealed he experienced onset of unilateral hearing loss two years prior.
His uncorrected visual acuity was 20/20 in the right eye and 20/800 in the left eye with no pinhole improvement. His pupils were equally round and reactive without a relative afferent pupillary defect. Confrontation visual field and extraocular motility testing were both normal, and the intraocular pressure was 15mm Hg in both eyes.
The anterior segment examination was normal in both eyes except for 1+ anterior chamber cell OS. Posterior segment findings were significant for trace vitreous cells with no vitreous haze in both eyes. Fundus photography (Figures 1 and 2) and OCT images (Figures 3 and 4) were obtained.
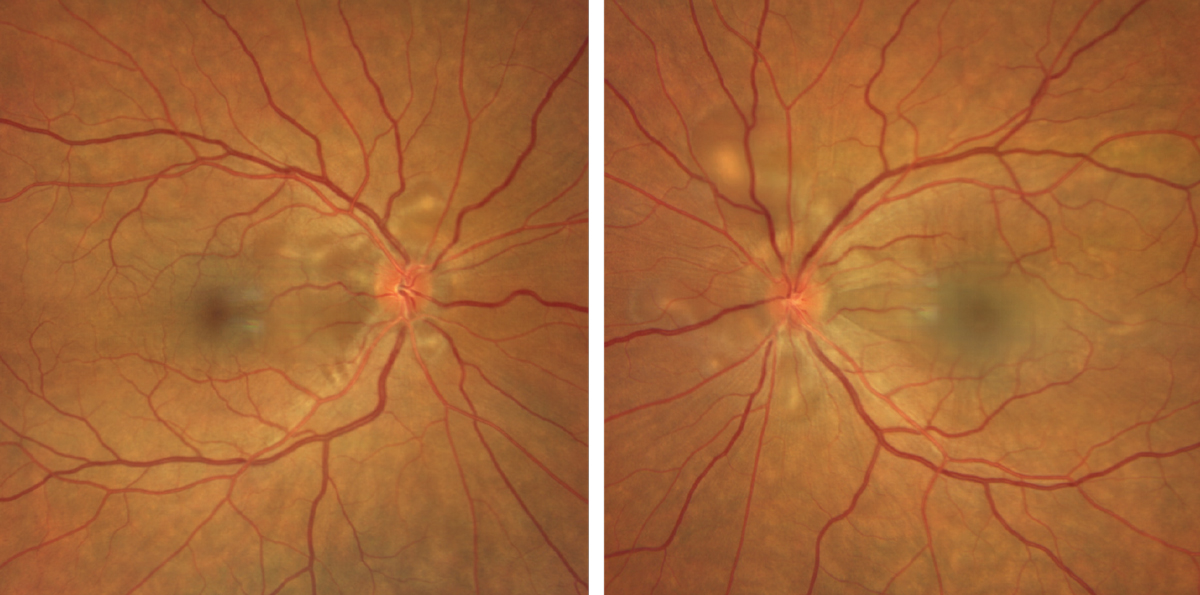 |
Figs. 1 and 2. Clarus fundus photography of the right eye (left) and left eye (right). Click image to enlarge. |
Take the Retina Quiz
1. Which of the following descriptions of the OCT retinal imaging is false?
a. There are multifocal neurosensory retinal detachments.
b. There are multifocal bacillary layer detachments.
c. There is choroidal thickening and infiltration.
d. All of the above are true.
2. What is the most likely diagnosis for this patient?
a. Endogenous endophthalmitis.
b. Sympathetic ophthalmia.
c. Toxoplasmosis.
d. Vogt-Koyanagi-Harada (VKH) disease.
3. What is the most appropriate next step in the management of this patient?
a. Hospital admission for blood cultures, intravenous anti-infectives and intravitreal anti-infectives.
b. Initiation of anti-tuberculum medications.
c. Initiation of anti-toxoplasmosis medications.
d. Initiation of immunosuppressive therapy.
4. Which of the following statements is true?
a. Sugiura sign describes depigmentation of the eyelids.
b. There is a strong association across most populations with HLA-B51.
c. “Sunset glow” describes the clinical picture of optic nerve pallor with peripapillary choroidal depigmentation, which appears as red-orange.
d. Patients with this condition often have a history of penetrating ocular trauma.
5. Which of the following is NOT a common complication of this patient’s condition?
a. Macular neovascularization.
b. Neovascular glaucoma.
c. Posterior subcapsular cataract.
d. Subretinal fibrosis.
For answers, see below.
Diagnosis
The fundus exam revealed focal, peripapillary, hypopigmented and granulomatous lesions around both optic nerves with overlying subretinal fluid. There is also clearly evident fluid underneath the macula in the left eye and fluid just nasal to the fovea in the right eye (Figures 1 and 2).
From the OCT images, we were able to anatomically visualize the serous neurosensory retinal detachments and confirm another interesting finding. Looking more closely you can see that the retinal pigmented epithelium (RPE) is not detached from Bruch’s membrane and, even more significantly, neither are the inner and outer photoreceptor segments (IS/OS junction). Instead, it appears the detachment is at the level of the external limiting membrane (ELM) and the IS/OS junction. These are referred to as bacillary layer detachments. OCT also shows choroidal thickening and infiltration in both eyes (Figures 3 and 4).
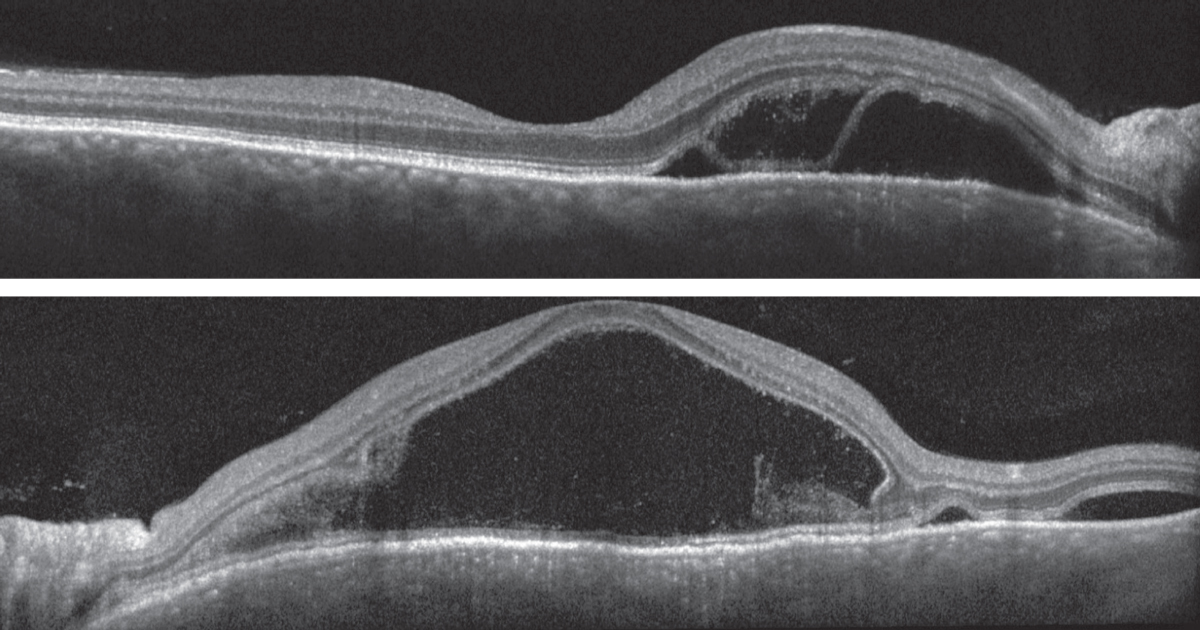 |
Figs. 3 and 4. Heidelberg spectral-domain OCT of the right eye (top) and left eye (bottom). Click image to enlarge. |
The clinical presentation and review of systems were most consistent with Vogt-Koyanagi-Harada (VKH) disease. The plan was to start 60mg of oral prednisone and prednisolone acetate 1% every two hours in both eyes; however, the patient was sent to have blood drawn right away to rule out infectious etiologies (syphilis and tuberculosis) prior to taking his first dose of prednisone, which came back negative. He was followed closely and demonstrated an adequate response to therapy with resolution of subretinal and intraretinal fluid; however, there was incomplete resolution of the choroidal thickening and infiltration. Vision in the right eye remained stable, and the left eye improved to 20/20.
Discussion
VKH disease is an immune-mediated condition against melanocyte-containing tissues (e.g., uvea, skin).1 Ophthalmic involvement typically presents as a bilateral, granulomatous, non-necrotizing posterior or panuveitis, and extraocular involvement may include dysacusis, poliosis, alopecia and vitiligo.2 Its incidence is variable as it tends to affect populations or races containing more pigment such as Asians, Hispanics, American Indians and Asian Indians.2 In the United States, VKH accounts for only 1% to 4% of all uveitis referrals.2 There may be a female predilection, and it often presents in the second to fifth decade of life.1,2
Classically, the disease progresses through four well-defined stages: (1) prodromal, (2) acute uveitic, (3) chronic-recurrent and (4) convalescent.2,3 The prodromal phase manifests as a nonspecific viral illness that lasts a few days. Symptoms can include malaise, headache, dizziness, fever, neck stiffness and auditory disturbances (tinnitus and dysacusis).2,3 The acute uveitic phase follows the prodromal phase with photophobia and blurred vision. Clinical findings of this stage include bilateral granulomatous posterior or panuveitis, choroidal thickening, multifocal exudative retinal detachments and optic nerve hyperemia and edema.2,3
While recurrent exudative retinal detachments are uncommon, the chronic recurrent phase typically involves a smoldering panuveitis with acute episodic flares of granulomatous anterior uveitis that may be resistant to corticosteroid therapy.2, 3 Complications of recurrent and smoldering inflammation include cataract formation, uveitic glaucoma, posterior synechiae, chorioretinal atrophy and subretinal neovascularization.2,3 The convalescent stage of the disease is predominantly characterized by depigmentation of the skin and choroid. This stage consists of poliosis, vitiligo, alopecia and most notably, the “sunset-glow” fundus, which describes a red-orange appearance of a pale optic nerve surrounded by peripapillary/juxtapapillary choroidal depigmentation.2,3
The exudative process in VKH classically causes detachment of the neurosensory retina from the RPE, as well as bacillary layer detachments (BALADs), which is what was seen in our patient.4,5 While BALADs were initially described as multilobulated serous retinal detachments due to the presence of subretinal fibrin and septae, advances in OCT technology have allowed better structural analysis.4,5 The term BALAD describes intraphotoreceptor splitting where the photoreceptor inner segments are detached from the outer segments and underlying ELM.4,5
Treatment
The mainstay of treatment for the acute uveitic phase is aggressive systemic and topical corticosteroid use.2 Initial treatment can be 60mg to 100mg per day of prednisone or a 200mg intravenous loading dose of methylprednisolone for three days with an oral taper; patients require a prolonged taper often for longer than six months.2 The chronic-recurrent phase of the disease is less responsive to corticosteroid therapy and often requires the use of other biologic or cytotoxic immunosuppressive agents (e.g., azathioprine, cyclophosphamide, mycophenolate mofetil and tacrolimus).2 Patients can often regain visual acuity of 20/40 or better barring any complications as previously mentioned.2
Retina Quiz Answers
1: d, 2: d, 3: d, 4: c, 5: b
Dr. Dunbar is the director of optometric services and optometry residency supervisor at the Bascom Palmer Eye Institute at the University of Miami. He is a founding member of the Optometric Glaucoma Society and the Optometric Retina Society. Dr. Dunbar is a consultant for Carl Zeiss Meditec, Allergan, Regeneron and Genentech.
Dr. Aboumourad currently practices at Bascom Palmer Eye Institute in Miami. He has no financial disclosures.
| 1. Freund KB, Sarraf D, Mieler WF, Yannuzzi L. The Retinal Atlas. 2017. 2. Schachat AP, Wilkinson CP, Hinton DR, et al. Ryan’s Retina, 6th Edition. Elsevier. 2018. 3. Gass JDM. Stereoscopic atlas of macular disease: a fundoscopic and angiographic presentation. January 1, 1970. 4. Ramtohul P, Engelbert M, Malclès A, et al. Bacillary layer detachment: multimodal imaging and histologic evidence of a novel optical coherence tomography terminology: Literature Review and Proposed Theory. Retina. 2021;41(11):2193-207. 5. Agarwal A, Freund KB, Kumar A, et al. Bacillary layer detachment in acute Vogt-koyanagi harada disease: a novel swept-source optical coherence tomography analysis. Retina 2021;41(4):774-83. |

