 |
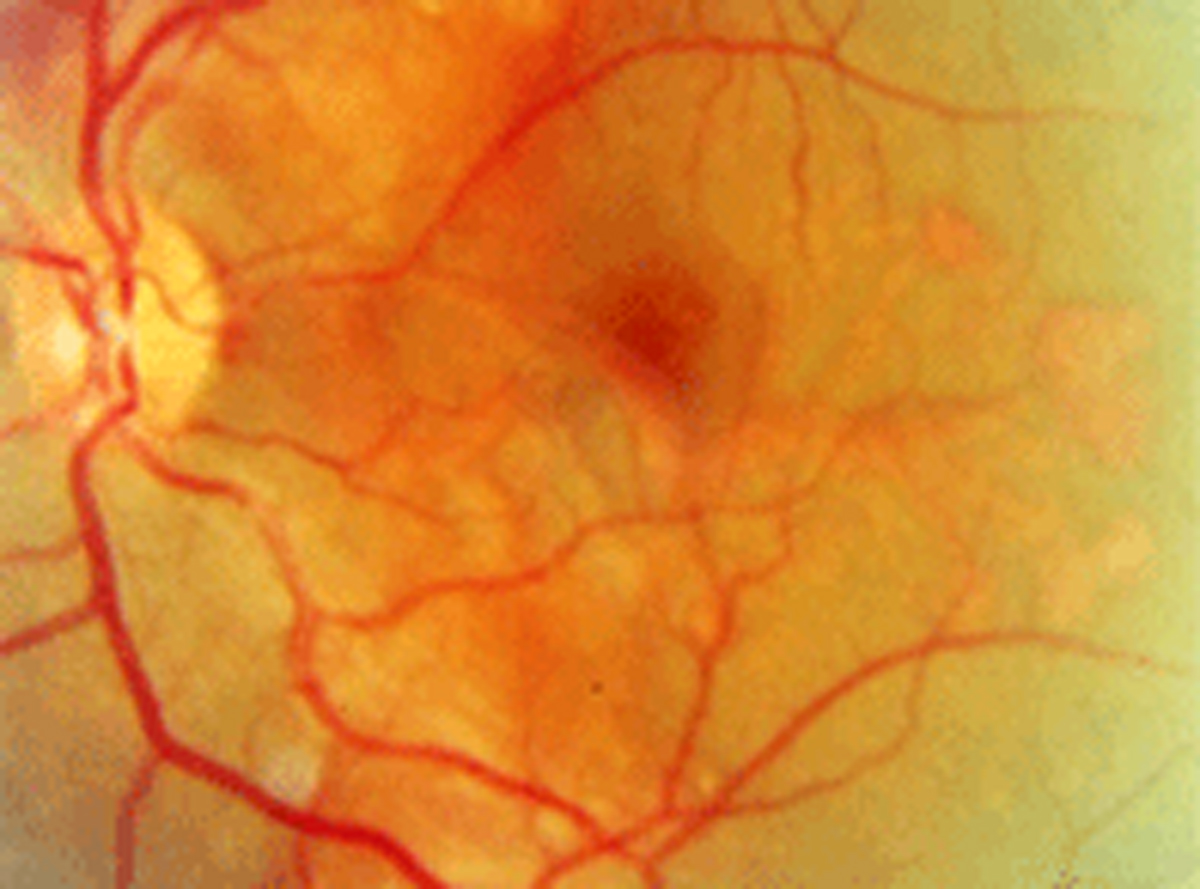
| Beyond four months, anti-VEGF therapy may no longer be effective at slowing progression of AMD-related peripapillary CNV. Photo: Diana L. Shechtman, OD. Click image to enlarge. |
A rare, vision-threatening form of choroidal neovascular membrane is called peripapillary choroidal neovascularization (CNV), which can produce minimal or no symptoms due to its extrafoveal location. Once detected, a handful of treatments are available to help slow disease progression and preserve vision, one of the most common being anti-VEGF injections. Researchers evaluated long-term outcomes of anti-VEGF agents on this population in a recent study, the largest and with the longest follow-up to-date on age-related macular degeneration (AMD)-related peripapillary CNV. They found that after four years, subsequent injections led to a significant deterioration in best-corrected visual acuity (BCVA).
The retrospective cohort study included 67 eyes of 66 patients (average age: 80.5) with AMD-related peripapillary CNV who were all treated with anti-VEGF injections on an as-needed basis. The mean follow-up period was 53.2 months. The researchers used inactivation index as one of the primary outcomes, which was calculated as the proportion of disease inactivity from the total follow-up time.
Throughout the first four years of follow-up, BCVA remained stable in most patients and anti-VEGF agents seemed to effectively preserve vision; however, by the final follow-up visit, BCVA had significantly decreased from baseline. The researchers also noted, “There was a statistically significant deterioration in BCVA with respect to baseline beginning in the fourth year of follow-up.”
A large majority of the eyes (88%) reached disease inactivation during follow-up (mean inactivation index: 0.38), which occurred for 49% of eyes after the first treatment cycle of three bevacizumab injections. This effect didn’t last, however. Of note: during follow-up, 20 eyes switched to ranibizumab and 11 to aflibercept.
“Of the eyes that reached disease inactivity, 85% had a recurrence during follow-up,” the researchers wrote. “The mean time to recurrence was nine months, while 35 eyes had recurrence less than three months after the first inactivation.” They noted that the estimated probability of recurrence was 0.59 and that this patient subset “had male preponderance and was significantly younger than patients with longer inactivation (median age: 79 vs. 84).”
The researchers made the following additional observations:
Baseline BCVA was a significant predictor of final BCVA.
Subretinal fluid at presentation was significantly associated with decreased inactivation index.
Worse baseline BCVA, subretinal fluid, pigment epithelium detachment, male sex and younger patient age were associated with increased risk for recurrence after the first inactivation.
The researchers concluded that although anti-VEGF seemed to effectively preserve vision within the first four years of follow-up, the prognosis of treatment began to dwindle thereafter. When caring for patients with AMD-related peripapillary CNV using anti-VEGF injections, be sure to perform careful follow-up to monitor ongoing response to treatment.
Stanescu N, Friehmann A, Nemet A, et al. Long-term outcomes of anti-vascular endothelial growth factor treatment in peripapillary choroidal neovascularisation due to age-related macular degeneration. Eye (Lond). May 17, 2022. [Epub ahead of print]. |

