 |
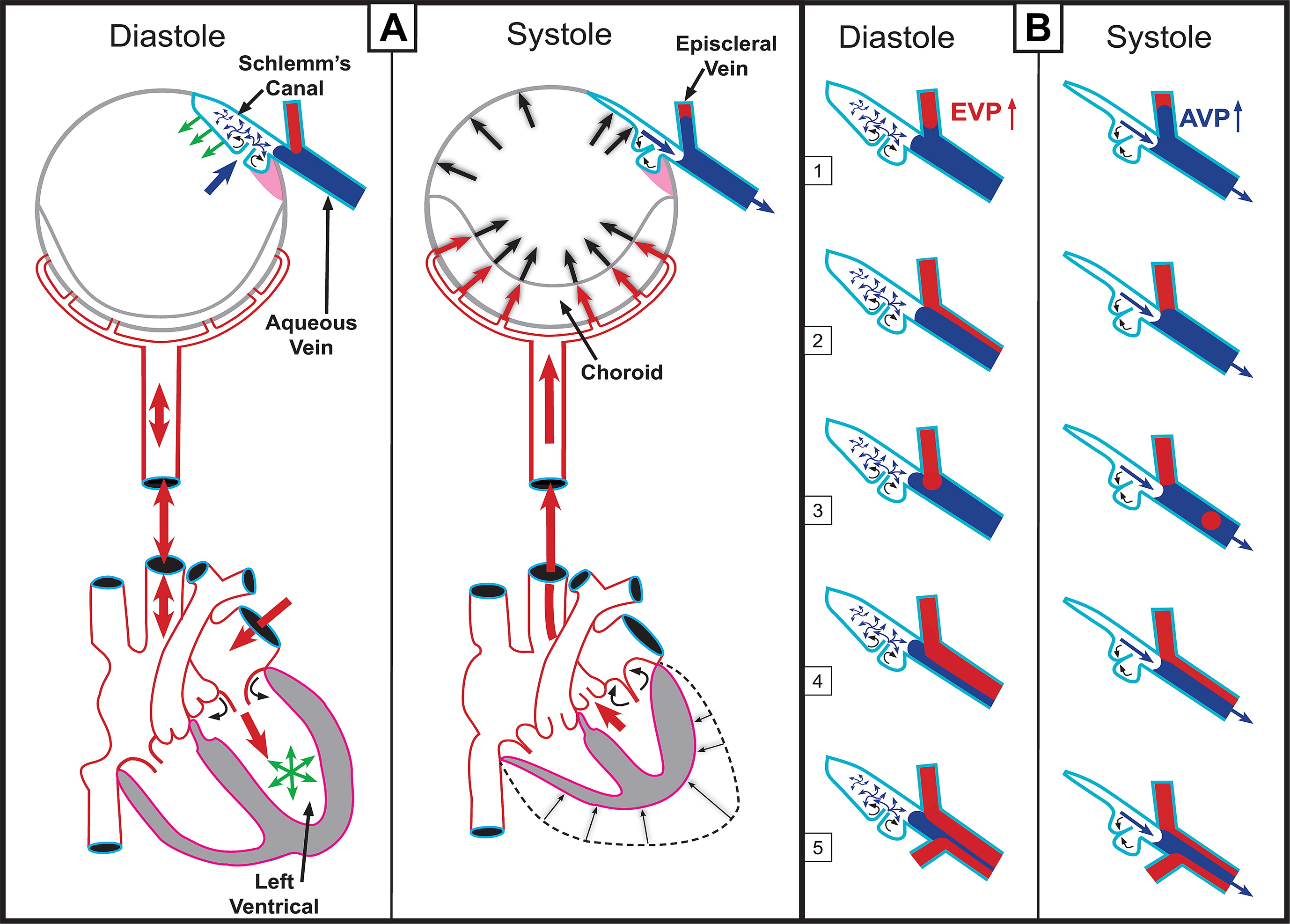
Ocular blood flow is an emerging factor in the course of glaucoma. Photo: Johnstone M et al. Experimental Eye Res. 2011; 92(5):318-327. Click image to enlarge. |
Elevated intraocular pressure is a recognized risk factor for glaucoma, and although it’s suspected that corneal biomechanical parameters may also correlate with the degree of glaucomatous damage and be predictive of future risk, research remains limited on that front. A new study published in the Journal of Glaucoma compared a range of metrics between eyes with asymmetric glaucoma and symmetric glaucoma and found some were markedly lower in the asymmetric group. “Comparing the eyes of patients with primary open-angle asymmetric glaucoma provides the opportunity to evaluate characteristics between eyes of the same patient,” the researchers explained in their paper.
A cohort of 45 subjects were divided into two groups, asymmetric glaucoma (32 eyes) and symmetric glaucoma (58 eyes). Metrics analyzed in the study included corneal hysteresis (CH), mean visual field deviation and ganglion cell complex thinning, among others. In the asymmetric group, the fellow eyes with more glaucomatous damage had lower CH, mean deviation and GCC thinning than the better eye. However, the symmetric group had no significantly different metrics between eyes. There was also no notable difference in IOP or central corneal thickness in either group, which the study authors say allowed a direct comparison of elastic and viscoelastic biomechanical parameters and removed all potential confounding variables.
Previous studies have indicated a relationship between CH and progressive glaucomatous damage due to the reduced capacity for damping, which may be associated with greater susceptibility to fluctuations in IOP. “Our finding that there was a significant difference between the eyes within the asymmetric group with worse [damage] having lower CH is consistent with the interpretation that low CH is associated with greater glaucomatous damage,” the researchers wrote. “It is important to note that this difference was found without the confounding influence of IOP or difference in central corneal thickness, providing powerful evidence of the association between lower CH and glaucomatous damage.” They hypothesized that CH, which is a viscoelastic parameter, could be more sensitive than elastic parameters in the development of glaucomatous damage.
This study also took a closer look at the role of vascular function in the disease process. As blood flows into the eye with each heartbeat, it creates a pulsatile waveform. A measurement called pulsatile ocular blood flow (POBF) reflects this dynamic but is difficult to measure clinically, so the study authors chose to estimate pulsatile ocular blood volume (POBV) to serve as a surrogate; a formula for calculating it combines IOP, ocular pulse amplitude and ocular rigidity. The researchers concluded POBF may indeed contribute to worse disease as other studies have suggested. Furthermore, its significant difference in those with asymmetric glaucoma provides proof that it may become a useful tool in diseases with compromised ocular circulation.
The authors noted the small sample size in their study as a limitation. “However, despite the small sample size, we did see significant differences between eyes in the viscoelastic metric CH and POBV as well as the ganglion cell complex and mean deviation,” they said. “Further investigation with a larger sample size may increase the power of the study to detect differences in elastic parameters.”
Harvey DH, Roberts CJ, Mahmoud, AM, Nuñez, FM, Ma Y, Fleming, GP. Biomechanical and vascular metrics between eyes of patients with asymmetric glaucoma and symmetric glaucoma. Journal of Glaucoma. January 9, 2024. [Epub ahead of print]. |

