 |
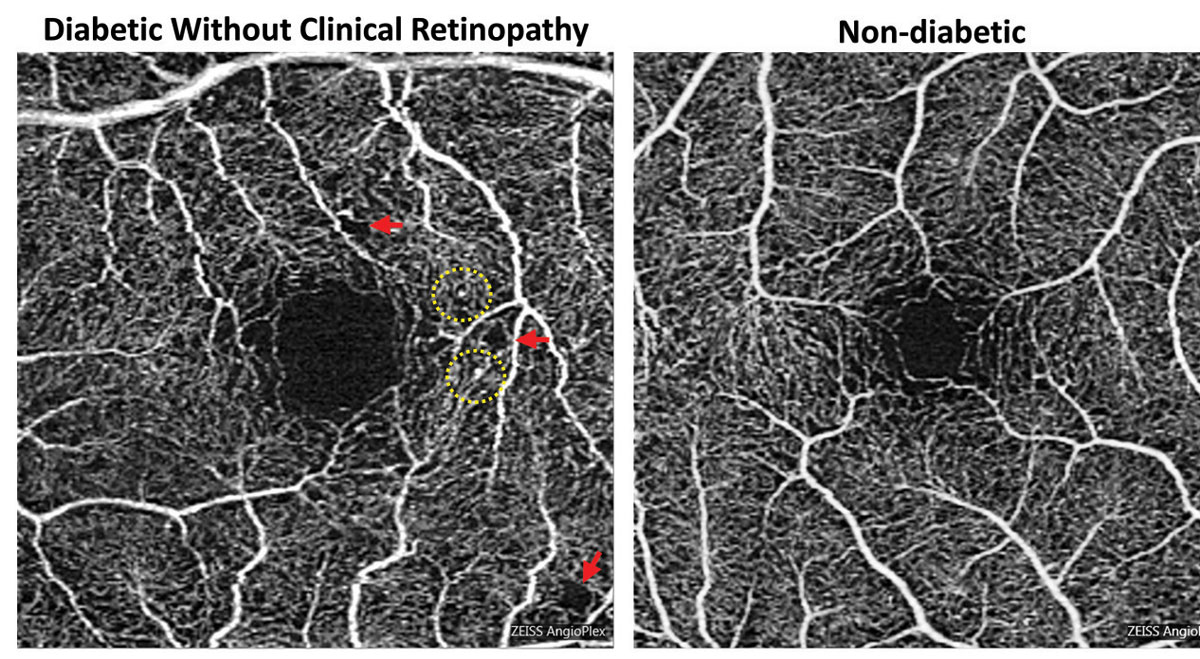
| On OCT-A, decreased retinal vessel density and perfusion density was associated with a high prevalence of diabetes and elevated fasting blood glucose concentration in a recent study. Photo: Carolyn Majcher, OD. Click image to enlarge. |
As optometrists play a crucial role in the early detection and management of ocular complications in patients with diabetes mellitus, understanding the systemic determinants influencing retinal microvascular alterations in these individuals is of utmost importance. Microvascular conditions in retinal vessels often reflect systemic or cardiovascular conditions due to their similar vascular scale and pathology. A recent study investigated the relationship between systemic factors and retinal microvascular parameters in patients with and without diabetes. The study design and primary findings are outlined below.
Data was derived from a large-sample cross-sectional study, known as the Kailuan Eye Study, in which 860 participants (ranging from 27 to 83 years old) underwent OCT angiography (OCT-A) to assess perfusion density (PD), vascular density (VD) and foveal avascular zone (FAZ) parameters of the superficial capillary plexus (SCP). Among the cohort, 449 individuals had diabetes with either no diabetic retinopathy or mild NPDR, and the remaining 411 participants did not have diabetes. Comprehensive systemic examinations were conducted to evaluate various risk factors, including age, sex, blood pressure, glucose and lipids.
The study findings revealed significant associations between diabetes and retinal microvascular alterations. Individuals with diabetes exhibited diminished PD and VD in the entire macular and parafoveal regions compared to those without diabetes. Furthermore, higher fasting plasma glucose (FPG) levels, longer axial length and elevated heart rate were correlated with reduced PD and VD in the macular region.
“Intriguingly, despite the inclusion of a multitude of systemic factors in our study, only FPG level was found to be significantly associated with retinal microvascular parameters after adjusting for age and axial length,” the study authors explained in their study, recently appearing in BMC Ophthalmology. “FPG levels have a distinct and direct negative correlation with retinal perfusion,” they stated, adding that this evidence “suggests that controlling blood glucose levels is a crucial therapeutic measure to ameliorate retinal ischemia and hypoxia and to prevent the onset of diabetic retinopathy in diabetic people.”
Notably, the study authors flagged hypertension and hyperlipidemia as important risk factors for atherosclerotic cardiovascular disease; however, these factors appeared to have no significant effect on retinal microvascular abnormalities.
Age was the only systemic factor that demonstrated an independent relationship to retinal vascular density in this study; however, the authors emphasized in their paper that comprehensive systemic examinations in diabetes patients are important given the observed associations between systemic factors such as glucose levels, axial length and heart rate with retinal microvascular alterations.
This study has several limitations. For one, the cross-sectional design limits the ability to establish causality. Secondly, the study population consisted of participants from a specific community, which could limit the generalizability of the findings. Other limitations include the lack of a control group, the exclusion of ocular parameters beyond those assessed on OCT-A and the lack of follow-up data that would have allowed researchers to assess the progression of retinal microvascular changes over time. Longitudinal studies with multiple time points would provide a more comprehensive understanding of the natural history and progression of diabetic retinopathy.
In conclusion, the authors summarize in their paper, “OCT-A can monitor early subclinical changes in retinal microvasculature, and regular OCT-A screening is beneficial for the diagnosis, classification and intervention of chronic systemic disease.”
Yao Y, Wang Q, Yang J, Yan Y, Wei W. Associations of retinal microvascular alterations with diabetes mellitus: an OCTA based cross-sectional study. BMC Ophthalmology. 2024;24:245. |

