 |
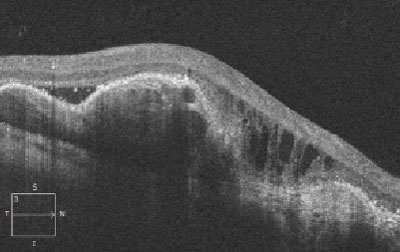
| In addition to using indocyanine green angiography, observing polypoidal lesions on OCT over time may help assess the risk for exudative conversion in patients with non-exudative polypoidal choroidal vasculopathy. Photo: Mark Dunbar, OD. Click image to enlarge. |
A subtype of neovascular AMD known as polypoidal choroidal vasculopathy (PCV) is characterized by polypoidal subretinal vascular lesions including branching neovascular network and nodular vascular complex. As the condition progresses and converts to exudation, patients face an increasing risk of serous and hemorrhagic detachment of the retinal pigment epithelium (RPE). Many patients with non-exudative PCV are also asymptomatic, adding to the importance of proper monitoring and disease classification.
Yet, limited knowledge exists regarding the incidence and risk factors of exudation in non-exudative PCV, which recently led a team of doctors to perform a small study to gain more clarity on the topic. In addition to assessing lesions using the gold-standard method, indocyanine green angiography, this study also used an imaging device owned by a growing number of optometrists today: OCT. They found that among 42 eyes of 40 patients (70% male; mean age 65) with treatment-naive non-exudative PCV, nearly half (46.4%) developed exudative conversion within five years, and the most significant biomarker for conversion was progressive protrusion of polypoidal lesions on OCT.
Kaplan-Meier estimates of exudation-free survival in the non-exudative PCV eyes were 79.8% after two years and 53.6% after five years. By the end of follow-up (54.3 ± 35.5 months), 23 eyes (54.8%) made up the conversion group, while 19 eyes (45.2%) were in the stable group. There were no differences in sex distribution, age or baseline BCVA between the two groups, but the conversion group did have a worse final BCVA than the stable group.
All eyes had branching neovascular network and polypoidal lesions at baseline, but contrary to some other reports, no difference was found in the number of polyps, size of largest polyp, area of branching neovascular network and location of polyps at baseline between the conversion and stable groups. During follow-up, nine eyes (22%) had a new occurrence of RPE protrusion, which happened at the same rate in both groups, though the conversion group had a higher proportion of eyes manifesting sequentially increased height of RPE protrusion (73.9% vs. 31.6% of the stable group) and heterogeneous hyporeflectivity within RPE protrusion (78.3% vs. 42.1%).
“As a main result of the current study, the progression of polypoidal lesions, which manifested as an increased height of RPE protrusion on OCT images, was a significant biomarker for predicting exudative conversion in non-exudative PCV,” the researchers wrote in their study, recently published in Retina. “The majority of the conversion group manifested exudation three years after the baseline. Furthermore, before conversion, it gives us an alarm of sequentially increased height of RPE protrusion at intervals of more than three months, which suggests that before the onset of exudative conversion, the clinician may have sufficient time to cope with it,” they explained.
In conclusion, the team proposes that observing RPE protrusion height over time on OCT may help to establish individualized monitoring and treatment strategies for patients with non-exudative PCV.
Son KY, Kim SJ, Kang SW, et al. Risk of exudation in eyes with non-exudative polypoidal choroidal vasculopathy. Retina. August 30, 2023. [Epub ahead of print]. |

