 |
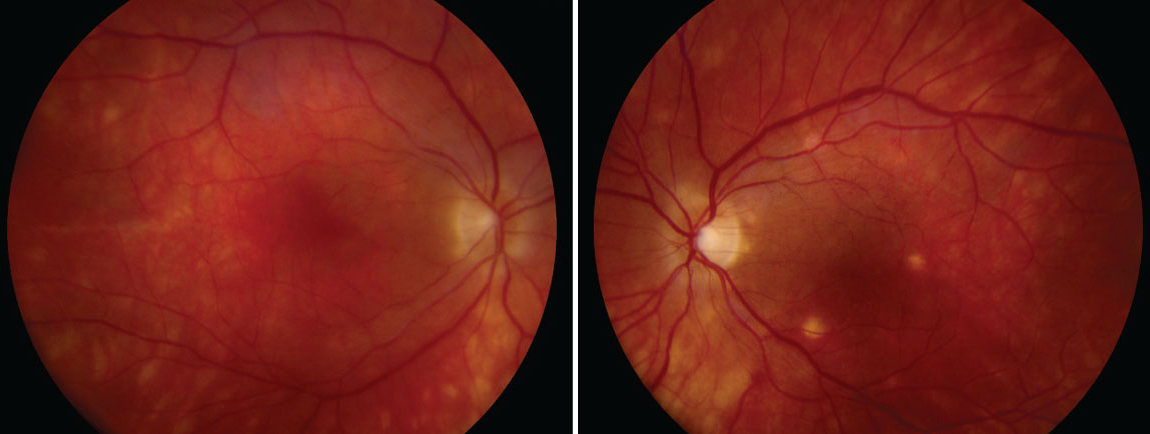
| Researchers recommend informing patients with uveitis about the modestly elevated risk of reactivation following COVID vaccination but do not consider previous bouts of uveitis to be a contraindication to vaccination, given its benefits overall. Photo: Ellen Butts, OD. Click image to enlarge. |
Cases of vaccine-associated uveitis have been identified in association with various vaccinations, including those preventative against COVID-19, and many of these involve cases of anterior uveitis. Studies have suggested the COVID vaccine may increase the risk of active non-infectious uveitis (NIU), but risk factors haven’t been identified. In a new retrospective population-based cohort study published in American Journal of Ophthalmology, researchers investigated the incidence and risk of NIU following COVID-19 vaccination compared to an unvaccinated, uninfected control group, and found an increased risk of NIU in females.
Included in the vaccine-exposed group were 5,185,153 individuals who received their first dose by Aug. 31, 2021. The study was conducted in Korea, where over 98% of the adult population had been vaccinated by March 2022. Accordingly, to arrive at a sufficiently sized control group, the researchers arbitrarily designated 2,671,891 subjects who received their first vaccine dose after Sept. 1, 2021 as the unexposed group and considered their data from the six months prior (March 1, 2021) to represent the unvaccinated period. The final tally of the unexposed, unvaccinated group was 2,680,164 individuals representing the control group.
An observed increase of non-infectious uveitis was identified up to 180 days post-vaccination, which suggests that vaccination tends to be more closely associated with a modest increase in non-anterior uveitis, as opposed to anterior or total uveitis. Subgroup analysis revealed increased risk of non-anterior uveitis in females, and previous non-infectious uveitis seemed to be the most significant risk factor.
Because this study analyzed the incidence and risk factors of NIU categorized into early- (within 60 days) vs. delayed-onset (between 60 and 180 days) and different parts of the uvea (total, anterior and non-anterior uveitis), the results could provide further insights into temporal and locational associations, the authors suggested.
“Previous studies have highlighted the temporal association between vaccination and the onset of NIU, usually within 30 days. In contrast, our study showed increased NIU in both early (within 60 days) and delayed onset (between 60 and 180 days), which may imply that delayed uveitis may be triggered by a different immunological mechanism,” the authors wrote in their paper. “We found that the risk of choroidal and retinal inflammation, rather than anterior uveitis, increased after COVID-19 vaccination. Therefore, molecular differences may exist between the anterior and posterior segments of the uvea that increase vulnerability to inflammation when exposed to different vaccines.”
Female sex, history of rheumatic autoimmune disease and previous non-infectious uveitis may increase the risk due to genetic factors or immune dysregulation due to preexisting immune-related disease. A history of non-infectious uveitis was found to be the most significant risk factor, with a hazard ratio ranging from 100 to 200, depending on the onset and location, the authors noted. Therefore, it may be plausible for eyecare providers “to warn patients with uveitis prior to vaccination about possible relapses and recommend shorter follow-up periods,” they explained. “However, considering the benefits of vaccination, previous non-infectious uveitis should not be considered a contraindication to COVID-19 vaccination. Moreover, further studies should be performed in patients with NIU to identify the risk factors for uveitis relapse after vaccination.”
It should be noted that this study excluded patients who had been diagnosed with NIU within two years prior to the index date and the unvaccinated cohort was selected from patient data that existed before the pandemic for historical comparison.
“Differences in findings regarding the association between COVID-19 vaccination and NIU may exist because our study population included 19 inactive NIU patients by excluding only those treated with corticosteroids within a year prior to the index date,” the authors explained in their AJO paper. “Additionally, the selection of an unvaccinated group during a different time frame may result in different population characteristics.”
Chang MS, Kim HR, Kim S, et al. Non-infectious uveitis risk after Coronavirus disease 2019 (COVID-19) vaccination: a nationwide retrospective cohort study. Amer J Ophthalmol. September 16, 2023. [Epub ahead of print.] |

